The need for a highly educated nursing workforce is in high demand due to the changing healthcare environment and the demographics of the U.S. population. Nurses require specialized knowledge and competencies to navigate the healthcare delivery system, such as leadership, research, integration of innovative technology and working in expanded roles and settings. These and other essential skill sets are vital for providing safe, high quality care. Nursing education and practice needs to move towards a patient-centered philosophy, higher standards for safe, quality care, with a stronger emphasis on information technology, scientific research, evidence-based practice, and interprofessional collaboration (Institute of Medicine [IOM], 2011).
The structure of America’s healthcare environment is continually evolving. Changing demographics brings about new cultures and practices. These cultural changes have brought about many questions about nursing’s ability to adapt yet maintain core values. How can essential nursing values hold up in the rapidly changing 21st century? In order to better understand the need for adaptation, it is important to understand certain changes that occurred since the 1960s.

Immigration and Globalization
In the 20th and 21st century, immigrants from Europe, Africa, Central America and Asia continued to settle in the U.S. to escape war, poverty, and oppression. America gave them the chance to live free and practice their cultural and religious beliefs without fear of outright persecution. People have always come to America to seek out a better life for themselves and their children.

One effect of globalization is increased mobility and the advent of international aid programs to facilitate movement throughout the world (Bruce, 2018). Modern America’s recent history was influenced by an immigration characterized by a mixture of religions, cultures, ethnicities, and races. Immigration from non-European areas has led to a wider variety of cultural integration becoming more pronounced in the U.S. (Bruce, 2018).
As a result of immigration and globalization, nurses must be committed to practice in a culturally congruent manner. According to the American Nurses Association (ANA, 2021) Standards of Professional Performance, Standard 9, Respectful and Equitable Practice, is fundamental to cultural humility and inclusiveness.
Providing culturally congruent care begins with creating a personal inventory of one’s values, beliefs, and cultural heritage. Knowing oneself helps nurses understand themselves better, they may find more similarities than differences when reflecting on one’s values and beliefs. Understanding the impact of social injustice and oppression on health helps nurses better understand their patients’ needs, leading to a more accurate assessment and plan of care.
Changing Demographics of the U.S.
As a result of immigration and globalization, the U.S. population has become more racially and culturally diverse. People are living longer with more chronic and complex illnesses as a result of technology and innovation. The following U.S. Census data (Colby & Ortman, 2015) projects an aging and more diverse U.S. population over the next 40 years:
- Increase from 319 million in 2014 to 417 million in 2060
- By 2030, one in five Americans is projected to be 65 and over
- By 2044, more than half of all Americans are projected to belong to a minority group (meaning any group other than non-Hispanic White)
- By 2060, nearly one in five of the nation’s total population is projected to be foreign born
Nurses need to be aware of these changes, and be prepared to understand the differences with morality, and prevent bias. Language translation is just one aspect of accommodating our unique patient needs. As yourself, what other barriers will occur as a result of increasing cultural diversity?
Chronic Disease and Risk Factors
The leading cause of death in the U.S. is transitioning from infectious, acute disease to chronic and degenerative illnesses (Centers for Disease Control and Prevention [CDC], 2003). In addition to higher rates of chronic disease, the aging population leads to severe disability later in life.
- Chronic disease (2015): (at least two diagnoses): 67.7% of those ≥ 65 (CDC, 2018b)
- Obesity (2018): 30.9% (CDC, 2020c)
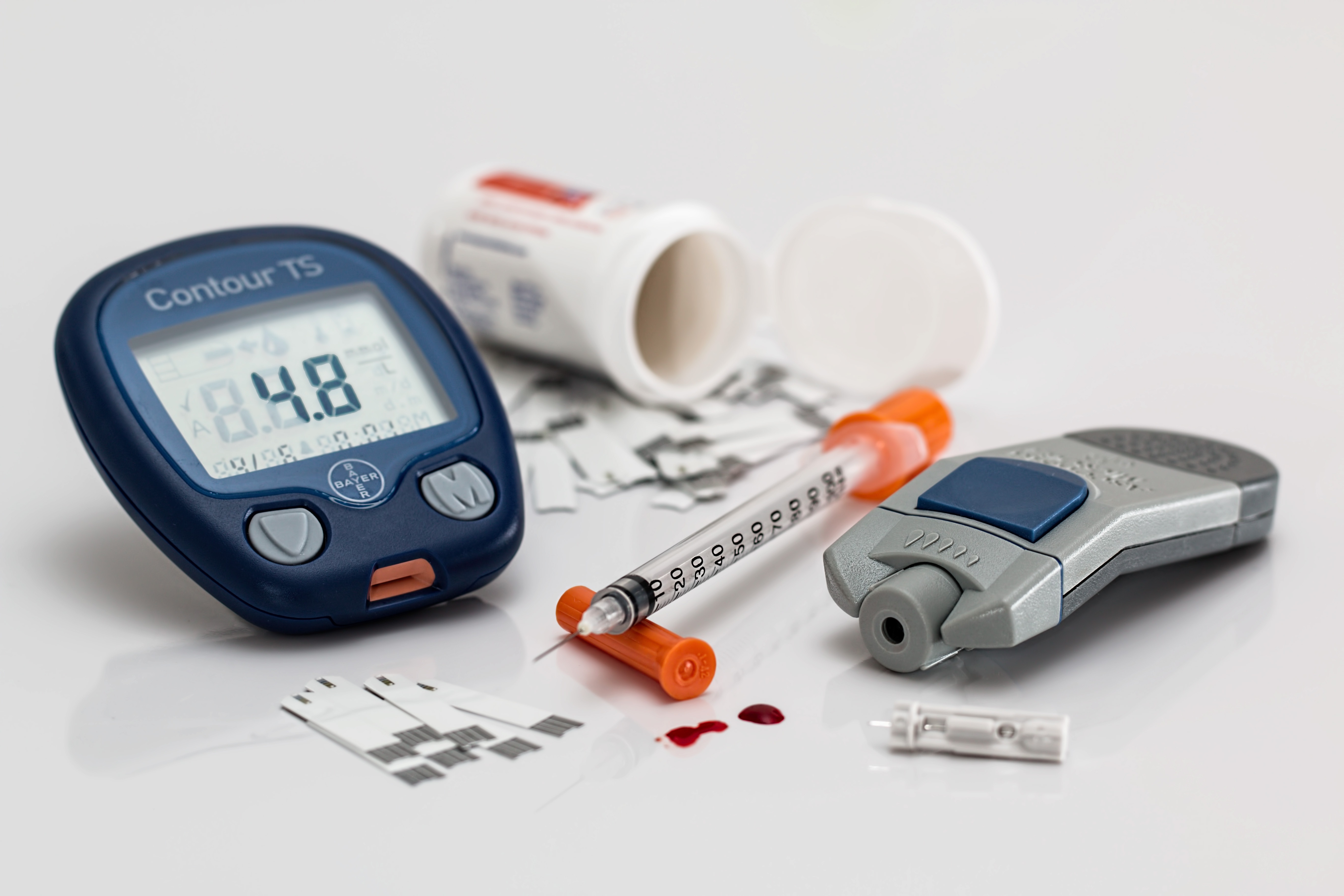
- Diabetes (2018)
- Type I and II, diagnosed and undiagnosed: 34.1 million
- Diagnosed: 26.8 million
- Undiagnosed: 7.3 million (CDC, 2020b)
- Type I and II, diagnosed and undiagnosed: 34.1 million
- Cardiovascular disease: 12.1% or 30.3 million (CDC, 2019)
- Arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia: 23% or 54 million (2015) (CDC, 2018b)
Chronic disease prevention and management requires individuals to modify risk factors that lead to chronic disease. The U.S. data below for adults aged 18 and older lists three modifiable risk factors for health promotion and disease prevention. Below are the current data for U.S. adults:
- Smoking:
- 16.6% (2018)(CDC, 2018b)
- 14% (2017)(CDC, 2018b)
- 15.5% (2016) (CDC, 2018b)
- 20.9% (2005) (CDC, 2020c)
- Exercise*(2017): 50% (CDC, 2020a)
- Diet (2017):
- 36%: eats less than one fruit/day
- 19%: eats less than one vegetable/day (CDC, 2020a)
* at least 150 minutes a week of moderate-intensity aerobic physical activity or 75 minutes a week of vigorous-intensity aerobic physical activity each week.
Technology and Healthcare
The 21st Century is known as the age of information technology. Healthcare has seen significant progress with technology and innovation over the past 25 years, especially since the Internet permeated almost every aspect of personal and work life. As a result, technology, specifically smartphones, has changed the way we interact with each other and how information is exchanged.
The following is a summary of the benefits of technological advances in healthcare:
- Improved effectiveness and efficiency
- Convenience (such as telehealth visit)
- Provide healthcare to rural locations, those with limited access to transportation (Huston, 2013)
- Data transparency
- Improved work environment, improved workflow
- Eliminates redundancy and duplication of documentation
- Reduces errors
- Eliminates interruptions for missing supplies, equipment, and medication
- Easier access to data
- Allows more time to spend with patients (as cited in Institute of Medicine, 2010)
Emerging Technologies
Huston (2013) cites the following emerging technologies that have a variety of benefits and challenges:
- Genetics and Genomics
- Prenatal/newborn screening
- Predictive value for disease or mutation
- Less Invasive and More Accurate Tools for Diagnostics and Treatment
- Blood tests diagnose heart disease compared to diagnostic angiograms
- Tattoos monitoring blood glucose without a finger stick
- 3-D Printing
- 3D printing of a prosthetic limbs, jaw, ear
- Robotics
- Nanotechnology to prevent and treat disease
- Pancreas pacemakers for diabetics
- Miniature cameras and microphones that can be wired into the brain, will exist, allowing blind people to see and deaf people to hear
- Biometrics
- Biometric signatures (fingerprints, retinal scan, voice recognition, etc.) improve confidentiality and security of data
- Electronic Healthcare Records (EHR)
- Captures data to improve safety and quality of care
- Computerized Physician/Provider Order; Entry (CPOE) and Clinical Decision Support
- Electronic orders lead to enhance healthcare decision-making and actions (pp. 3-10)

3-D printing prosthetic hand

biometrics: eye mapping
The Human Connection
Huston (2013) explains the core challenges with technology, such as retaining the human element in practice (discussed below). Balancing the high cost of technology with the benefits is significant for the entire healthcare system, including hospitals, clinics, pharmacies, etc. Initial training of the nursing workforce with ongoing competency is costly, compelling leadership to find ways to contain these high costs. Lastly, ensuring technology is used in an ethical way has become increasingly important with the advent of lifesaving technology and even integration of robots. Do patient want to check into their provider’s office by speaking to a robot? Technology can bring about fear of the unknown when a new treatment is touted to cure disease beyond what is normally possible.

Technology can improve the quality of one’s life in many circumstances, though it can also bring on ethical questions. Is it worth prolonging one’s life to the point where quality is reduced or no longer exists?
Healthcare as we know it today is heavily reliant on technology to streamline care, though innovation has isolated nurses and other healthcare staff from interacting with patients in a number of ways. Consider self-registration and automatic check-in stations. As much as technology can save time and be more cost-effective, the loss of the personal touch can negatively impact healthcare. The loss of a human connection, social cues, and rich conversations negatively impact care by inadvertently fragmenting care and a disconnecting the patient from the healthcare team (Thorne et al., 2005).
Innovation increases the risk of losing sight of the core values that are the inherent in the nursing profession (Lee, Laux, & Robitaille, 2018). Nurses are challenged to fit in the time to nurture the human connection with patients, coworkers and other support staff. Nurses need to find creative, personal ways outside of technology to show caring and compassion, especially in stressful work environments like healthcare settings.
How often do patients receive full eye contact during an intake? Technology can save time and resources, though it can cause patients to feel like a number (Thorne et al., 2005).
Medical breakthroughs, technological advances, and experimental treatments can also give patients a false sense of security that disease can be cured (Lee et al., 2018). For example, patients may struggle to know when it is the right time to end cancer treatments. Innovative treatments can offer endless treatment options, requiring nurses to assist patients with these important decisions. Providing the caring and compassion outside the veil of technology should encourage nurses to be fully present.
The Essentials
As we can see, healthcare has undergone a multitude of changes, which . The Essentials include competencies that prepare nurses to work in complex healthcare environments. Additionally, nurses must be competent in information technology systems so they can gather evidence to guide practice (American Association of Colleges of Nursing [AACN], 2021).
Information literacy is crucial for the future of nursing, and healthcare system as a whole. McNeil et al. (2006) explain the integration of evidence-based practice, interprofessional care coordination, and use of electronic health records rely on information management and technology to contain costs and improve safety.
Additional information about the Essentials can be found at the AACN website.
The Changing Role of Nursing Practice
The foundational report by the IOM (2010), The Future of Nursing: Leading Change, Advancing Health, asserts that nurses are poised to play a critical role in transforming the healthcare system to meet the increasing demands for safe, high-quality, accessible, and cost-effective healthcare. In order to provide this high level of care, nurses at all levels of care must understand how they can be involved in this momentous change. Such changes require nurses to consider a new way of thinking and practicing. Instead of providing care with the focus on the disease process, nurses need to view the bigger picture, and transition towards promoting care across the continuum. The patient’s family must be considered within the community setting to ensure the needed supports and resources are accessible, leading to health and well-being (Salmond & Echevarria, 2017).
Salmond and Echevarria (2017) review four core areas of nursing practice necessary for improving care:
- Wellness (The Essentials, Domain 3)
- Person- and family-centered care (The Essentials, Domain 2)
- Care coordination (The Essentials, Domain 6)
- Data analytics; focus on outcomes and improvement (The Essentials, Domain 8)
Nurses need to transition care from an illness-based focus to one that incorporates prevention and wellness approaches (Salmond & Echevarria, 2017). Prevention strategies must begin at home and within the community in order to maintain health and well-being. Nurses are uniquely positioned to educate patients and their families about the role of health promotion and self-care in preventing acute illnesses.
Social Determinants of Health
Thinking beyond the acute care event is an integral part of a complete patient assessment. Considering the factors leading up to an acute illness are often a combination of both social and environmental triggers. These triggers, such as living in a safe neighborhood and health literacy, will influence nurses’ decision-making throughout the entire nursing process. See Table 1 for a list of environmental and social triggers, known as social and physical determinants of health (SDOH) (U.S. Department of Health and Human Services, 2020). Nurses must be cognizant of the changing demographics of the U.S. population when considering the determinants of health throughout all aspects of care.
Table 1 depicts the social and physical determinants of health
| Social Determinants | Environmental (physical) Determinants |
|---|---|
| Availability of resources to meet daily needs (e.g., safe housing and local food markets) | Natural environment, such as green space (e.g., trees and grass) or weather (e.g., climate change) |
| Access to educational, economic, and job opportunities | Built environment, such as buildings, sidewalks, bike lanes, and roads |
| Access to health care services | Worksites, schools, and recreational settings |
| Quality of education and job training | Housing and community design |
| Availability of community-based resources in support of community living and opportunities for recreational and leisure-time activities | Exposure to toxic substances and other physical hazards |
| Transportation options | Physical barriers, especially for people with disabilities |
| Public safety | Aesthetic elements (e.g., good lighting, trees, and benches) |
| Social support | |
| Social norms and attitudes (e.g., discrimination, racism, and distrust of government) | |
| Exposure to crime, violence, and social disorder (e.g., presence of trash and lack of cooperation in a community) | |
| Socioeconomic conditions (e.g., concentrated poverty and the stressful conditions that accompany it) | |
| Residential segregation | |
| Language/Literacy | |
| Access to mass media and emerging technologies (e.g., cell phones, the Internet, and social media) | |
| Culture | |
(U.S. Department of Health and Human Services, 2018)
SDOH and other concepts found in The Essentials (Diversity, Equity, and Inclusion; Ethics; and Health Policy) are interconnected, and together they can explain how well (or how poorly) a community, state, or country addresses the factors that impact health. For example, people living in rural areas may have less access to education (public school) leading to lower reading and health literacy rates. Knowing education is a key factor in attaining employment, financial stability, and ultimately optimal health outcomes, community or government leaders must address barriers to education. Health policy can address the inequities found in certain populations to ensure everyone has equal and equitable access to education.
Alvarado (2019) studied the relationship between the neighborhoods children grew up and whether it led to adult obesity. The results found children were more likely to be obese during adulthood when exposed to disadvantaged neighborhoods. While nurses need to instill the public health message of curbing obesity in adulthood, awareness of factors that lead to obesity must be considered. Alvarado (2019) states policy needs to focus on the processes that occur during childhood development, such as the state of the neighborhoods where children live and play.

Person- and family-centered care intersects with care coordination as a result of nursing’s strong emphasis on providing holistic care. Delivering holistic care ensures an unwavering focus on the needs of the patient and family (American Nurses Association, 2012). Advocating for and embracing patients and families as active partners in their care is integral for providing quality care. Nurses need to acknowledge that patients’ input is invaluable and must include patients and families as partners in decision-making. When patients and families are part of the decision-making process, they become more vested in their care, they are incentivized to meet self-care needs and follow through with disease prevention activities (Salmond & Echevarria, 2017).
An essential part of reaching health outcomes and improved quality of care relies on nurses understanding the care they provide. Nurses need to recognize that data influences their care, and healthcare delivery as a whole. Understanding key metrics, such as hospital readmissions or infection rates, is an example of how data informs practice. Nurses need to use data to improve practice at the individual level, though understanding the data at the population level is how practice evolves (Salmond & Echevarria, 2017). Through collaboration with other disciplines and researchers, nurses are able to use data to reach new goals to improve outcomes and quality, reduce cost, and more.
Upholding Nurses Values
As the configuration of America’s communities change as a result of globalization, nurses must stay true to their core values of caring for others for altruistic reasons. Many nurses enter the profession due to their desire to help and care for others in need. Nurses are faced with providing care to a changing demographic, having to understand and respect the most vulnerable patients with human dignity (Bruce, 2018).
Nurses are caring for patients who fled their countries due to violence, sexual assault, and religious persecution, hoping to live in America’s communities. Patients are relying on nurses to protect them, care for them without bias or prejudice, both emotionally and physically. Nurses have the power to ensure quality care to these vulnerable patients. Nurses are no stranger to advocating for patients’ needs, though practice must continually adapt in this changing environment.
Bruce (2018) writes about the importance of nurses upholding and actively maintaining the core values of why nurses entered this beloved and amazing profession. Providing care in a selfless, noble way is still a primary mission of nurses, and when these values are combined with a caring approach, nurses are well prepared to support diversity and meet patients’ healthcare needs. Increasing tolerance will lead nurses to embrace the differences that are encountered when patients have opposing beliefs, different ethnicities, races, religion, sexual orientation, and citizenship. Caring for vulnerable populations requires the core value of caring for every kind of patient to be a prominent aspect of all nursing practice.
In order to ensure healthcare delivery offers safe, high quality, and cost-effective care, nurses must assume diverse roles and achieve a wide variety of competencies (knowledge, skills, abilities). Nurses play a central role in transforming care at the individual level, and when nurses work together, change can occur broadly, for broader community. Below is a brief review of the necessary roles and competencies of the nursing workforce for the 21st Century:
- Change agent
- Lead and inspire others towards change
- Disease prevention and wellness
- Prevention of adverse events (such as hospital-acquired infections)
- Clinical knowledge grounded in evidence
- Respond to data and track trends
- Focus on excellence and the patient experience
- Responsiveness to determinants of health
- Management of chronic conditions
- Care coordination across the continuum
- Patient-centric, patient as a partner
- Team-based, collaborative care
- Optimize the use of innovative technology
- Patient and family advocacy to promote:
- health promotion
- navigation of a complex healthcare systems
Candela Citations
- Transitions to Professional Nursing Practice. Authored by: Jamie Murphy. Provided by: SUNY Delhi. Located at: https://courses.lumenlearning.com/suny-delhi-professionalnursing. License: CC BY: Attribution
