Stress is a process whereby an individual perceives and responds to events appraised as overwhelming or threatening to one’s well-being. The scientific study of how stress and emotional factors impact health and well-being is called health psychology, a field devoted to studying the general impact of psychological factors on health. While there are circumstances in which stress can be good, we know that stress can have serious negative consequences on the body.
Stressors can be chronic (long term) or acute (short term), and can include traumatic events, significant life changes, daily hassles, and situations in which people are frequently exposed to challenging and unpleasant events. Many potential stressors include events or situations that require us to make changes in our lives, such as a divorce or moving to a new residence. Thomas Holmes and Richard Rahe developed the Social Readjustment Rating Scale (SRRS) to measure stress by assigning a number of life change units to life events that typically require some adjustment, including positive events. Although the SRRS has been criticized on a number of grounds, extensive research has shown that the accumulation of many LCUs is associated with increased risk of illness. Many potential stressors also include daily hassles, which are minor irritations and annoyances that can build up over time. In addition, jobs that are especially demanding, offer little control over one’s working environment, or involve unfavorable working conditions can lead to job strain, thereby setting the stage for job burnout.
What is Stress?
The term stress as it relates to the human condition first emerged in scientific literature in the 1930s, but it did not enter the popular vernacular until the 1970s (Lyon, 2012). Today, we often use the term loosely in describing a variety of unpleasant feeling states; for example, we often say we are stressed out when we feel frustrated, angry, conflicted, overwhelmed, or fatigued. Despite the widespread use of the term, stress is a fairly vague concept that is difficult to define with precision.
Video 1. What is Stress?
A useful way to conceptualize stress is to view it as a process whereby an individual perceives and responds to events that he appraises as overwhelming or threatening to his well-being (Lazarus & Folkman, 1984). A critical element of this definition is that it emphasizes the importance of how we appraise—that is, judge—demanding or threatening events (often referred to as stressors); these appraisals, in turn, influence our reactions to such events. Two kinds of appraisals of a stressor are especially important in this regard: primary and secondary appraisals. A primary appraisal involves judgment about the degree of potential harm or threat to well-being that a stressor might entail. A stressor would likely be appraised as a threat if one anticipates that it could lead to some kind of harm, loss, or other negative consequence; conversely, a stressor would likely be appraised as a challenge if one believes that it carries the potential for gain or personal growth. For example, an employee who is promoted to a leadership position would likely perceive the promotion as a much greater threat if she believed the promotion would lead to excessive work demands than if she viewed it as an opportunity to gain new skills and grow professionally. Similarly, a college student on the cusp of graduation may face the change as a threat or a challenge (Figure 1).

Figure 1. Graduating from college and entering the workforce can be viewed as either a threat (loss of financial support) or a challenge (opportunity for independence and growth). (credit: Timothy Zanker)
The perception of a threat triggers a secondary appraisal: judgment of the options available to cope with a stressor, as well as perceptions of how effective such options will be (Lyon, 2012) (Figure 2). As you may recall from what you learned about self-efficacy, an individual’s belief in his ability to complete a task is important (Bandura, 1994). A threat tends to be viewed as less catastrophic if one believes something can be done about it (Lazarus & Folkman, 1984). Imagine that two middle-aged women, Robin and Maria, perform breast self-examinations one morning and each woman notices a lump on the lower region of her left breast. Although both women view the breast lump as a potential threat (primary appraisal), their secondary appraisals differ considerably. In considering the breast lump, some of the thoughts racing through Robin’s mind are, “Oh my God, I could have breast cancer! What if the cancer has spread to the rest of my body and I cannot recover? What if I have to go through chemotherapy? I’ve heard that experience is awful! What if I have to quit my job? My husband and I won’t have enough money to pay the mortgage. Oh, this is just horrible…I can’t deal with it!” On the other hand, Maria thinks, “Hmm, this may not be good. Although most times these things turn out to be benign, I need to have it checked out. If it turns out to be breast cancer, there are doctors who can take care of it because the medical technology today is quite advanced. I’ll have a lot of different options, and I’ll be just fine.” Clearly, Robin and Maria have different outlooks on what might turn out to be a very serious situation: Robin seems to think that little could be done about it, whereas Maria believes that, worst case scenario, a number of options that are likely to be effective would be available. As such, Robin would clearly experience greater stress than would Maria.

Figure 2. When encountering a stressor, a person judges its potential threat (primary appraisal) and then determines if effective options are available to manage the situation. Stress is likely to result if a stressor is perceived as extremely threatening or threatening with few or no effective coping options available.
To be sure, some stressors are inherently more stressful than others in that they are more threatening and leave less potential for variation in cognitive appraisals (e.g., objective threats to one’s health or safety). Nevertheless, appraisal will still play a role in augmenting or diminishing our reactions to such events (Everly & Lating, 2002).
If a person appraises an event as harmful and believes that the demands imposed by the event exceed the available resources to manage or adapt to it, the person will subjectively experience a state of stress. In contrast, if one does not appraise the same event as harmful or threatening, she is unlikely to experience stress. According to this definition, environmental events trigger stress reactions by the way they are interpreted and the meanings they are assigned. In short, stress is largely in the eye of the beholder: it’s not so much what happens to you as it is how you respond (Selye, 1976).
Try It
Responses to Stress
When stressed, we may have a number of physiological, psychological, and behavioral responses. The type of response may depend on the stressor and our appraisal.
Cannon and the Fight-or-Flight Response
Imagine that you are hiking in the beautiful mountains of Colorado on a warm and sunny spring day. At one point during your hike, a large, frightening-looking black bear appears from behind a stand of trees and sits about 50 yards from you. The bear notices you, sits up, and begins to lumber in your direction. In addition to thinking, “This is definitely not good,” a constellation of physiological reactions begins to take place inside you. Prompted by a deluge of epinephrine (adrenaline) and norepinephrine (noradrenaline) from your adrenal glands, your pupils begin to dilate. Your heart starts to pound and speeds up, you begin to breathe heavily and perspire, you get butterflies in your stomach, and your muscles become tense, preparing you to take some kind of direct action. Cannon proposed that this reaction, which he called the fight-or-flight response, occurs when a person experiences very strong emotions—especially those associated with a perceived threat (Cannon, 1932). During the fight-or-flight response, the body is rapidly aroused by activation of both the sympathetic nervous system and the endocrine system (Figure 7). This arousal helps prepare the person to either fight or flee from a perceived threat.

Figure 3. Fight or flight is a physiological response to a stressor.
According to Cannon, the fight-or-flight response is a built-in mechanism that assists in maintaining homeostasis—an internal environment in which physiological variables such as blood pressure, respiration, digestion, and temperature are stabilized at levels optimal for survival. Thus, Cannon viewed the fight-or-flight response as adaptive because it enables us to adjust internally and externally to changes in our surroundings, which is helpful in species survival.
Selye and the General Adaptation Syndrome

Figure 4. Hans Selye specialized in research about stress. In 2009, his native Hungary honored his work with this stamp, released in conjunction with the 2nd annual World Conference on Stress.
Another important early contributor to the stress field was Hans Selye, mentioned earlier. He would eventually become one of the world’s foremost experts in the study of stress (Figure 8). As a young assistant in the biochemistry department at McGill University in the 1930s, Selye was engaged in research involving sex hormones in rats. Although he was unable to find an answer for what he was initially researching, he incidentally discovered that when exposed to prolonged negative stimulation (stressors)—such as extreme cold, surgical injury, excessive muscular exercise, and shock—the rats showed signs of adrenal enlargement, thymus and lymph node shrinkage, and stomach ulceration. Selye realized that these responses were triggered by a coordinated series of physiological reactions that unfold over time during continued exposure to a stressor. These physiological reactions were nonspecific, which means that regardless of the type of stressor, the same pattern of reactions would occur. What Selye discovered was the general adaptation syndrome, the body’s nonspecific physiological response to stress.
The general adaptation syndrome, shown in Figure 9, consists of three stages: (1) alarm reaction, (2) stage of resistance, and (3) stage of exhaustion (Selye, 1936; 1976). Alarm reaction describes the body’s immediate reaction upon facing a threatening situation or emergency, and it is roughly analogous to the fight-or-flight response described by Cannon. During an alarm reaction, you are alerted to a stressor, and your body alarms you with a cascade of physiological reactions that provide you with the energy to manage the situation. A person who wakes up in the middle of the night to discover her house is on fire, for example, is experiencing an alarm reaction.

Figure 5. The three stages of Selye’s general adaptation syndrome are shown in this graph. Prolonged stress ultimately results in exhaustion.
If exposure to a stressor is prolonged, the organism will enter the stage of resistance. During this stage, the initial shock of alarm reaction has worn off and the body has adapted to the stressor. Nevertheless, the body also remains on alert and is prepared to respond as it did during the alarm reaction, although with less intensity. For example, suppose a child who went missing is still missing 72 hours later. Although the parents would obviously remain extremely disturbed, the magnitude of physiological reactions would likely have diminished over the 72 intervening hours due to some adaptation to this event.
If exposure to a stressor continues over a longer period of time, the stage of exhaustion ensues. At this stage, the person is no longer able to adapt to the stressor: the body’s ability to resist becomes depleted as physical wear takes its toll on the body’s tissues and organs. As a result, illness, disease, and other permanent damage to the body—even death—may occur. If a missing child still remained missing after three months, the long-term stress associated with this situation may cause a parent to literally faint with exhaustion at some point or even to develop a serious and irreversible illness.
In short, Selye’s general adaptation syndrome suggests that stressors tax the body via a three-phase process—an initial jolt, subsequent readjustment, and a later depletion of all physical resources—that ultimately lays the groundwork for serious health problems and even death. It should be pointed out, however, that this model is a response-based conceptualization of stress, focusing exclusively on the body’s physical responses while largely ignoring psychological factors such as appraisal and interpretation of threats. Nevertheless, Selye’s model has had an enormous impact on the field of stress because it offers a general explanation for how stress can lead to physical damage and, thus, disease. As we shall discuss later, prolonged or repeated stress has been implicated in development of a number of disorders such as hypertension and coronary artery disease.
Try It
The Physiological Basis of Stress
What goes on inside our bodies when we experience stress? The physiological mechanisms of stress are extremely complex, but they generally involve the work of two systems—the sympathetic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis. When a person first perceives something as stressful (Selye’s alarm reaction), the sympathetic nervous system triggers arousal via the release of adrenaline from the adrenal glands. Release of these hormones activates the fight-or-flight responses to stress, such as accelerated heart rate and respiration. At the same time, the HPA axis, which is primarily endocrine in nature, becomes especially active, although it works much more slowly than the sympathetic nervous system. In response to stress, the hypothalamus (one of the limbic structures in the brain) releases corticotrophin-releasing factor, a hormone that causes the pituitary gland to release adrenocorticotropic hormone (ACTH) (Figure 10). The ACTH then activates the adrenal glands to secrete a number of hormones into the bloodstream; an important one is cortisol, which can affect virtually every organ within the body. Cortisol is commonly known as a stress hormone and helps provide that boost of energy when we first encounter a stressor, preparing us to run away or fight. However, sustained elevated levels of cortisol weaken the immune system.

Figure 6. This diagram shows the functioning of the hypothalamic-pituitary-adrenal (HPA) axis. The hypothalamus activates the pituitary gland, which in turn activates the adrenal glands, increasing their secretion of cortisol.
In short bursts, this process can have some favorable effects, such as providing extra energy, improving immune system functioning temporarily, and decreasing pain sensitivity. However, extended release of cortisol—as would happen with prolonged or chronic stress—often comes at a high price. High levels of cortisol have been shown to produce a number of harmful effects. For example, increases in cortisol can significantly weaken our immune system (Glaser & Kiecolt-Glaser, 2005), and high levels are frequently observed among depressed individuals (Geoffroy, Hertzman, Li, & Power, 2013). In summary, a stressful event causes a variety of physiological reactions that activate the adrenal glands, which in turn release epinephrine, norepinephrine, and cortisol. These hormones affect a number of bodily processes in ways that prepare the stressed person to take direct action, but also in ways that may heighten the potential for illness.
When stress is extreme or chronic, it can have profoundly negative consequences. For example, stress often contributes to the development of certain psychological disorders, including post-traumatic stress disorder, major depressive disorder, and other serious psychiatric conditions. Additionally, we noted earlier that stress is linked to the development and progression of a variety of physical illnesses and diseases. For example, researchers in one study found that people injured during the September 11, 2001, World Trade Center disaster or who developed post-traumatic stress symptoms afterward later suffered significantly elevated rates of heart disease (Jordan, Miller-Archie, Cone, Morabia, & Stellman, 2011). Another investigation yielded that self-reported stress symptoms among aging and retired Finnish food industry workers were associated with morbidity 11 years later. This study also predicted the onset of musculoskeletal, nervous system, and endocrine and metabolic disorders (Salonen, Arola, Nygård, & Huhtala, 2008). Another study reported that male South Korean manufacturing employees who reported high levels of work-related stress were more likely to catch the common cold over the next several months than were those employees who reported lower work-related stress levels (Park et al., 2011). Later, you will explore the mechanisms through which stress can produce physical illness and disease.
Try It
Stressors
Good Stress?
Although stress carries a negative connotation, at times it may be of some benefit. Stress can motivate us to do things in our best interests, such as study for exams, visit the doctor regularly, exercise, and perform to the best of our ability at work. Indeed, Selye (1974) pointed out that not all stress is harmful. He argued that stress can sometimes be a positive, motivating force that can improve the quality of our lives. This kind of stress, which Selye called eustress (from the Greek eu = “good”), is a good kind of stress associated with positive feelings, optimal health, and performance. A moderate amount of stress can be beneficial in challenging situations. For example, athletes may be motivated and energized by pregame stress, and students may experience similar beneficial stress before a major exam. Indeed, research shows that moderate stress can enhance both immediate and delayed recall of educational material. Male participants in one study who memorized a scientific text passage showed improved memory of the passage immediately after exposure to a mild stressor as well as one day following exposure to the stressor (Hupbach & Fieman, 2012).
Increasing one’s level of stress will cause performance to change in a predictable way. As shown in Figure 3, as stress increases, so do performance and general well-being (eustress); when stress levels reach an optimal level (the highest point of the curve), performance reaches its peak. A person at this stress level is colloquially at the top of his game, meaning he feels fully energized, focused, and can work with minimal effort and maximum efficiency. But when stress exceeds this optimal level, it is no longer a positive force—it becomes excessive and debilitating, or what Selye termed distress (from the Latin dis = “bad”). People who reach this level of stress feel burned out; they are fatigued, exhausted, and their performance begins to decline. If the stress remains excessive, health may begin to erode as well (Everly & Lating, 2002).

Figure 7. As the stress level increases from low to moderate, so does performance (eustress). At the optimal level (the peak of the curve), performance has reached its peak. If stress exceeds the optimal level, it will reach the distress region, where it will become excessive and debilitating, and performance will decline (Everly & Lating, 2002).
The Prevalence of Stress
Stress is everywhere and, as shown in Figure 4, it has been on the rise over the last several years. Each of us is acquainted with stress—some are more familiar than others. In many ways, stress feels like a load you just can’t carry—a feeling you experience when, for example, you have to drive somewhere in a crippling blizzard, when you wake up late the morning of an important job interview, when you run out of money before the next pay period, and before taking an important exam for which you realize you are not fully prepared.

Figure 8. Nearly half of U.S. adults indicated that their stress levels have increased over the last five years (Neelakantan, 2013).
Stress is an experience that evokes a variety of responses, including those that are physiological (e.g., accelerated heart rate, headaches, or gastrointestinal problems), cognitive (e.g., difficulty concentrating or making decisions), and behavioral (e.g., drinking alcohol, smoking, or taking actions directed at eliminating the cause of the stress). Although stress can be positive at times, it can have deleterious health implications, contributing to the onset and progression of a variety of physical illnesses and diseases (Cohen & Herbert, 1996).
The scientific study of how stress and other psychological factors impact health falls within the realm of health psychology, a subfield of psychology devoted to understanding the importance of psychological influences on health, illness, and how people respond when they become ill (Taylor, 1999). Health psychology emerged as a discipline in the 1970s, a time during which there was increasing awareness of the role behavioral and lifestyle factors play in the development of illnesses and diseases (Straub, 2007). In addition to studying the connection between stress and illness, health psychologists investigate issues such as why people make certain lifestyle choices (e.g., smoking or eating unhealthy food despite knowing the potential adverse health implications of such behaviors). Health psychologists also design and investigate the effectiveness of interventions aimed at changing unhealthy behaviors. Perhaps one of the more fundamental tasks of health psychologists is to identify which groups of people are especially at risk for negative health outcomes, based on psychological or behavioral factors. For example, measuring differences in stress levels among demographic groups and how these levels change over time can help identify populations who may have an increased risk for illness or disease.
Figure 5 depicts the results of three national surveys in which several thousand individuals from different demographic groups completed a brief stress questionnaire; the surveys were administered in 1983, 2006, and 2009 (Cohen & Janicki-Deverts, 2012). All three surveys demonstrated higher stress in women than in men. Unemployed individuals reported high levels of stress in all three surveys, as did those with less education and income; retired persons reported the lowest stress levels. However, from 2006 to 2009 the greatest increase in stress levels occurred among men, Whites, people aged 45–64, college graduates, and those with full-time employment. One interpretation of these findings is that concerns surrounding the 2008–2009 economic downturn (e.g., threat of or actual job loss and substantial loss of retirement savings) may have been especially stressful to White, college-educated, employed men with limited time remaining in their working careers.

Try It
For an individual to experience stress, he must first encounter a potential stressor. In general, stressors can be placed into one of two broad categories: chronic and acute. Chronic stressors include events that persist over an extended period of time, such as caring for a parent with dementia, long-term unemployment, or imprisonment. Acute stressors involve brief focal events that sometimes continue to be experienced as overwhelming well after the event has ended, such as falling on an icy sidewalk and breaking your leg (Cohen, Janicki-Deverts, & Miller, 2007). Whether chronic or acute, potential stressors come in many shapes and sizes. They can include major traumatic events, significant life changes, daily hassles, as well as other situations in which a person is regularly exposed to threat, challenge, or danger.
Traumatic Events
Some stressors involve traumatic events or situations in which a person is exposed to actual or threatened death or serious injury. Stressors in this category include exposure to military combat, threatened or actual physical assaults (e.g., physical attacks, sexual assault, robbery, childhood abuse), terrorist attacks, natural disasters (e.g., earthquakes, floods, hurricanes), and automobile accidents. Men, non-Whites, and individuals in lower socioeconomic status (SES) groups report experiencing a greater number of traumatic events than do women, Whites, and individuals in higher SES groups (Hatch & Dohrenwend, 2007). Some individuals who are exposed to stressors of extreme magnitude develop post-traumatic stress disorder (PTSD): a chronic stress reaction characterized by experiences and behaviors that may include intrusive and painful memories of the stressor event, jumpiness, persistent negative emotional states, detachment from others, angry outbursts, and avoidance of reminders of the event (American Psychiatric Association [APA], 2013).
Life Changes
Most stressors that we encounter are not nearly as intense as the ones described above. Many potential stressors we face involve events or situations that require us to make changes in our ongoing lives and require time as we adjust to those changes. Examples include death of a close family member, marriage, divorce, and moving (Figure 1).

Figure 9. Some fairly typical life events, such as moving, can be significant stressors. Even when the move is intentional and positive, the amount of resulting change in daily life can cause stress. (credit: “Jellaluna”/Flickr)
In the 1960s, psychiatrists Thomas Holmes and Richard Rahe wanted to examine the link between life stressors and physical illness, based on the hypothesis that life events requiring significant changes in a person’s normal life routines are stressful, whether these events are desirable or undesirable. They developed the Social Readjustment Rating Scale (SRRS), consisting of 43 life events that require varying degrees of personal readjustment (Holmes & Rahe, 1967). Many life events that most people would consider pleasant (e.g., holidays, retirement, marriage) are among those listed on the SRRS; these are examples of eustress. Holmes and Rahe also proposed that life events can add up over time, and that experiencing a cluster of stressful events increases one’s risk of developing physical illnesses.
In developing their scale, Holmes and Rahe asked 394 participants to provide a numerical estimate for each of the 43 items; each estimate corresponded to how much readjustment participants felt each event would require. These estimates resulted in mean value scores for each event—often called life change units (LCUs) (Rahe, McKeen, & Arthur, 1967). The numerical scores ranged from 11 to 100, representing the perceived magnitude of life change each event entails. Death of a spouse ranked highest on the scale with 100 LCUs, and divorce ranked second highest with 73 LCUs. In addition, personal injury or illness, marriage, and job termination also ranked highly on the scale with 53, 50, and 47 LCUs, respectively. Conversely, change in residence (20 LCUs), change in eating habits (15 LCUs), and vacation (13 LCUs) ranked low on the scale (Table 1). Minor violations of the law ranked the lowest with 11 LCUs. To complete the scale, participants checked yes for events experienced within the last 12 months. LCUs for each checked item are totaled for a score quantifying the amount of life change. Agreement on the amount of adjustment required by the various life events on the SRRS is highly consistent, even cross-culturally (Holmes & Masuda, 1974).
| Life event | Life change units |
|---|---|
| Death of a close family member | 63 |
| Personal injury or illness | 53 |
| Dismissal from work | 47 |
| Change in financial state | 38 |
| Change to different line of work | 36 |
| Outstanding personal achievement | 28 |
| Beginning or ending school | 26 |
| Change in living conditions | 25 |
| Change in working hours or conditions | 20 |
| Change in residence | 20 |
| Change in schools | 20 |
| Change in social activities | 18 |
| Change in sleeping habits | 16 |
| Change in eating habits | 15 |
| Minor violation of the law | 11 |
Extensive research has demonstrated that accumulating a high number of life change units within a brief period of time (one or two years) is related to a wide range of physical illnesses (even accidents and athletic injuries) and mental health problems (Monat & Lazarus, 1991; Scully, Tosi, & Banning, 2000). In an early demonstration, researchers obtained LCU scores for U.S. and Norwegian Navy personnel who were about to embark on a six-month voyage. A later examination of medical records revealed positive (but small) correlations between LCU scores prior to the voyage and subsequent illness symptoms during the ensuing six-month journey (Rahe, 1974). In addition, people tend to experience more physical symptoms, such as backache, upset stomach, diarrhea, and acne, on specific days in which self-reported LCU values are considerably higher than normal, such as the day of a family member’s wedding (Holmes & Holmes, 1970).
The Social Readjustment Rating Scale (SRRS) provides researchers a simple, easy-to-administer way of assessing the amount of stress in people’s lives, and it has been used in hundreds of studies (Thoits, 2010). Despite its widespread use, the scale has been subject to criticism. First, many of the items on the SRRS are vague; for example, death of a close friend could involve the death of a long-absent childhood friend that requires little social readjustment (Dohrenwend, 2006). In addition, some have challenged its assumption that undesirable life events are no more stressful than desirable ones (Derogatis & Coons, 1993). However, most of the available evidence suggests that, at least as far as mental health is concerned, undesirable or negative events are more strongly associated with poor outcomes (such as depression) than are desirable, positive events (Hatch & Dohrenwend, 2007). Perhaps the most serious criticism is that the scale does not take into consideration respondents’ appraisals of the life events it contains. As you recall, appraisal of a stressor is a key element in the conceptualization and overall experience of stress. Being fired from work may be devastating to some but a welcome opportunity to obtain a better job for others. The SRRS remains one of the most well-known instruments in the study of stress, and it is a useful tool for identifying potential stress-related health outcomes (Scully et al., 2000).
Link to Learning
Go to this site to complete the SRRS scale and determine the total number of LCUs you have experienced over the last year.
Try It
Hassles
Potential stressors do not always involve major life events. Daily hassles—the minor irritations and annoyances that are part of our everyday lives (e.g., rush hour traffic, lost keys, obnoxious coworkers, inclement weather, arguments with friends or family)—can build on one another and leave us just as stressed as life change events (Figure 2) (Kanner, Coyne, Schaefer, & Lazarus, 1981).

Figure 10. Daily commutes, whether (a) on the road or (b) via public transportation, can be hassles that contribute to our feelings of everyday stress. (credit a: modification of work by Jeff Turner; credit b: modification of work by “epSos.de”/Flickr)
Researchers have demonstrated that the frequency of daily hassles is actually a better predictor of both physical and psychological health than are life change units. In a well-known study of San Francisco residents, the frequency of daily hassles was found to be more strongly associated with physical health problems than were life change events (DeLongis, Coyne, Dakof, Folkman, & Lazarus, 1982). In addition, daily minor hassles, especially interpersonal conflicts, often lead to negative and distressed mood states (Bolger, DeLongis, Kessler, & Schilling, 1989). Cyber hassles that occur on social media may represent a new source of stress. In one investigation, undergraduates who, over a 10-week period, reported greater Facebook-induced stress (e.g., guilt or discomfort over rejecting friend requests and anger or sadness over being unfriended by another) experienced increased rates of upper respiratory infections, especially if they had larger social networks (Campisi et al., 2012). Clearly, daily hassles can add up and take a toll on us both emotionally and physically.
Other Stressors
Stressors can include situations in which one is frequently exposed to challenging and unpleasant events, such as difficult, demanding, or unsafe working conditions. Although most jobs and occupations can at times be demanding, some are clearly more stressful than others (Figure 3). For example, most people would likely agree that a firefighter’s work is inherently more stressful than that of a florist. Equally likely, most would agree that jobs containing various unpleasant elements, such as those requiring exposure to loud noise (heavy equipment operator), constant harassment and threats of physical violence (prison guard), perpetual frustration (bus driver in a major city), or those mandating that an employee work alternating day and night shifts (hotel desk clerk), are much more demanding—and thus, more stressful—than those that do not contain such elements. Table 2 lists several occupations and some of the specific stressors associated with those occupations (Sulsky & Smith, 2005).

Figure 11. (a) Police officers and (b) firefighters hold high stress occupations. (credit a: modification of work by Australian Civil-Military Centre; credit b: modification of work by Andrew Magill)
| Occupation | Stressors Specific to Occupation (Sulsky & Smith, 2005) |
|---|---|
| Police officer | physical dangers, excessive paperwork, red tape, dealing with court system, coworker and supervisor conflict, lack of support from the public |
| Firefighter | uncertainty over whether a serious fire or hazard awaits after an alarm |
| Social worker | little positive feedback from jobs or from the public, unsafe work environments, frustration in dealing with bureaucracy, excessive paperwork, sense of personal responsibility for clients, work overload |
| Teacher | Excessive paperwork, lack of adequate supplies or facilities, work overload, lack of positive feedback, vandalism, threat of physical violence |
| Nurse | Work overload, heavy physical work, patient concerns (dealing with death and medical concerns), interpersonal problems with other medical staff (especially physicians) |
| Emergency medical worker | Unpredictable and extreme nature of the job, inexperience |
| Air traffic controller | Little control over potential crisis situations and workload, fear of causing an accident, peak traffic situations, general work environment |
| Clerical and secretarial work | Little control over job mobility, unsupportive supervisors, work overload, lack of perceived control |
| Managerial work | Work overload, conflict and ambiguity in defining the managerial role, difficult work relationships |
Although the specific stressors for these occupations are diverse, they seem to share two common denominators: heavy workload and uncertainty about and lack of control over certain aspects of a job. Both of these factors contribute to job strain, a work situation that combines excessive job demands and workload with little discretion in decision making or job control (Karasek & Theorell, 1990). Clearly, many occupations other than the ones listed in Table 2 involve at least a moderate amount of job strain in that they often involve heavy workloads and little job control (e.g., inability to decide when to take breaks). Such jobs are often low-status and include those of factory workers, postal clerks, supermarket cashiers, taxi drivers, and short-order cooks. Job strain can have adverse consequences on both physical and mental health; it has been shown to be associated with increased risk of hypertension (Schnall & Landsbergis, 1994), heart attacks (Theorell et al., 1998), recurrence of heart disease after a first heart attack (Aboa-Éboulé et al., 2007), significant weight loss or gain (Kivimäki et al., 2006), and major depressive disorder (Stansfeld, Shipley, Head, & Fuhrer, 2012). A longitudinal study of over 10,000 British civil servants reported that workers under 50 years old who earlier had reported high job strain were 68% more likely to later develop heart disease than were those workers under 50 years old who reported little job strain (Chandola et al., 2008).
Some people who are exposed to chronically stressful work conditions can experience job burnout, which is a general sense of emotional exhaustion and cynicism in relation to one’s job (Maslach & Jackson, 1981). Job burnout occurs frequently among those in human service jobs (e.g., social workers, teachers, therapists, and police officers). Job burnout consists of three dimensions. The first dimension is exhaustion—a sense that one’s emotional resources are drained or that one is at the end of her rope and has nothing more to give at a psychological level. Second, job burnout is characterized by depersonalization: a sense of emotional detachment between the worker and the recipients of his services, often resulting in callous, cynical, or indifferent attitudes toward these individuals. Third, job burnout is characterized by diminished personal accomplishment, which is the tendency to evaluate one’s work negatively by, for example, experiencing dissatisfaction with one’s job-related accomplishments or feeling as though one has categorically failed to influence others’ lives through one’s work.
Job strain appears to be one of the greatest risk factors leading to job burnout, which is most commonly observed in workers who are older (ages 55–64), unmarried, and whose jobs involve manual labor. Heavy alcohol consumption, physical inactivity, being overweight, and having a physical or lifetime mental disorder are also associated with job burnout (Ahola, et al., 2006). In addition, depression often co-occurs with job burnout. One large-scale study of over 3,000 Finnish employees reported that half of the participants with severe job burnout had some form of depressive disorder (Ahola et al., 2005). Job burnout is often precipitated by feelings of having invested considerable energy, effort, and time into one’s work while receiving little in return (e.g., little respect or support from others or low pay) (Tatris, Peeters, Le Blanc, Schreurs, & Schaufeli, 2001).
As an illustration, consider CharlieAnn, a nursing assistant who worked in a nursing home. CharlieAnn worked long hours for little pay in a difficult facility. Her supervisor was domineering, unpleasant, and unsupportive; he was disrespectful of CharlieAnn’s personal time, frequently informing her at the last minute she must work several additional hours after her shift ended or that she must report to work on weekends. CharlieAnn had very little autonomy at her job. She had little say in her day-to-day duties and how to perform them, and she was not permitted to take breaks unless her supervisor explicitly told her that she could. CharlieAnn did not feel as though her hard work was appreciated, either by supervisory staff or by the residents of the home. She was very unhappy over her low pay, and she felt that many of the residents treated her disrespectfully.
After several years, CharlieAnn began to hate her job. She dreaded going to work in the morning, and she gradually developed a callous, hostile attitude toward many of the residents. Eventually, she began to feel as though she could no longer help the nursing home residents. CharlieAnn’s absenteeism from work increased, and one day she decided that she had had enough and quit. She now has a job in sales, vowing never to work in nursing again.
Finally, our close relationships with friends and family—particularly the negative aspects of these relationships—can be a potent source of stress. Negative aspects of close relationships can include adverse exchanges and conflicts, lack of emotional support or confiding, and lack of reciprocity. All of these can be overwhelming, threatening to the relationship, and thus stressful. Such stressors can take a toll both emotionally and physically. A longitudinal investigation of over 9,000 British civil servants found that those who at one point had reported the highest levels of negative interactions in their closest relationship were 34% more likely to experience serious heart problems (fatal or nonfatal heart attacks) over a 13–15 year period, compared to those who experienced the lowest levels of negative interaction (De Vogli, Chandola & Marmot, 2007).
Try It
Responses to Stress
As stress researcher Robert Sapolsky (1998) describes,
stress-related disease emerges, predominantly, out of the fact that we so often activate a physiological system that has evolved for responding to acute physical emergencies, but we turn it on for months on end, worrying about mortgages, relationships, and promotions. (p. 6)
The stress response, as noted earlier, consists of a coordinated but complex system of physiological reactions that are called upon as needed. These reactions are beneficial at times because they prepare us to deal with potentially dangerous or threatening situations (for example, recall our old friend, the fearsome bear on the trail). However, health is affected when physiological reactions are sustained, as can happen in response to ongoing stress. A number of studies have demonstrated that stress weakens the functioning of the immune system. Cardiovascular disorders are serious medical conditions that have been consistently shown to be influenced by stress and negative emotions, such as anger, negative affectivity, and depression. Other psychophysiological disorders that are known to be influenced by stress and emotional factors include asthma and tension headaches.
Psychophysiological Disorders
If the reactions that compose the stress response are chronic or if they frequently exceed normal ranges, they can lead to cumulative wear and tear on the body, in much the same way that running your air conditioner on full blast all summer will eventually cause wear and tear on it. For example, the high blood pressure that a person under considerable job strain experiences might eventually take a toll on his heart and set the stage for a heart attack or heart failure. Also, someone exposed to high levels of the stress hormone cortisol might become vulnerable to infection or disease because of weakened immune system functioning (McEwen, 1998).
Physical disorders or diseases whose symptoms are brought about or worsened by stress and emotional factors are called psychophysiological disorders. The physical symptoms of psychophysiological disorders are real and they can be produced or exacerbated by psychological factors (hence the psycho and physiological in psychophysiological). A list of frequently encountered psychophysiological disorders is provided in Table 1.
| Type of Psychophysiological Disorder | Examples |
|---|---|
| Cardiovascular | hypertension, coronary heart disease |
| Gastrointestinal | irritable bowel syndrome |
| Respiratory | asthma, allergy |
| Musculoskeletal | low back pain, tension headaches |
| Skin | acne, eczema, psoriasis |
In addition to stress itself, emotional upset and certain stressful personality traits have been proposed as potential contributors to ill health. Franz Alexander (1950), an early-20th-century psychoanalyst and physician, once postulated that various diseases are caused by specific unconscious conflicts. For example, he linked hypertension to repressed anger, asthma to separation anxiety, and ulcers to an unconscious desire to “remain in the dependent infantile situation—to be loved and cared for” (Alexander, 1950, p. 102). Although hypertension does appear to be linked to anger (as you will learn below), Alexander’s assertions have not been supported by research. Years later, Friedman and Booth-Kewley (1987), after statistically reviewing 101 studies examining the link between personality and illness, proposed the existence of disease-prone personality characteristics, including depression, anger/hostility, and anxiety. Indeed, a study of over 61,000 Norwegians identified depression as a risk factor for all major disease-related causes of death (Mykletun et al., 2007). In addition, neuroticism—a personality trait that reflects how anxious, moody, and sad one is—has been identified as a risk factor for chronic health problems and mortality (Ploubidis & Grundy, 2009).
Before we discuss two kinds of psychophysiological disorders about which a great deal is known: cardiovascular disorders and asthma, it is necessary to turn our attention to a discussion of the immune system—one of the major pathways through which stress and emotional factors can lead to illness and disease.
Stress and the Immune System
In a sense, the immune system is the body’s surveillance system. It consists of a variety of structures, cells, and mechanisms that serve to protect the body from invading toxins and microorganisms that can harm or damage the body’s tissues and organs. When the immune system is working as it should, it keeps us healthy and disease free by eliminating bacteria, viruses, and other foreign substances that have entered the body (Everly & Lating, 2002).
Immune System Errors
Sometimes, the immune system will function erroneously. For example, sometimes it can go awry by mistaking your body’s own healthy cells for invaders and repeatedly attacking them. When this happens, the person is said to have an autoimmune disease, which can affect almost any part of the body. How an autoimmune disease affects a person depends on what part of the body is targeted. For instance, rheumatoid arthritis, an autoimmune disease that affects the joints, results in joint pain, stiffness, and loss of function. Systemic lupus erythematosus, an autoimmune disease that affects the skin, can result in rashes and swelling of the skin. Grave’s disease, an autoimmune disease that affects the thyroid gland, can result in fatigue, weight gain, and muscle aches (National Institute of Arthritis and Musculoskeletal and Skin Diseases [NIAMS], 2012).
In addition, the immune system may sometimes break down and be unable to do its job. This situation is referred to as immunosuppression, the decreased effectiveness of the immune system. When people experience immunosuppression, they become susceptible to any number of infections, illness, and diseases. For example, acquired immune deficiency syndrome (AIDS) is a serious and lethal disease that is caused by human immunodeficiency virus (HIV), which greatly weakens the immune system by infecting and destroying antibody-producing cells, thus rendering a person vulnerable to any of a number of opportunistic infections (Powell, 1996).
Stressors and Immune Function
The question of whether stress and negative emotional states can influence immune function has captivated researchers for over three decades, and discoveries made over that time have dramatically changed the face of health psychology (Kiecolt-Glaser, 2009). Psychoneuroimmunology is the field that studies how psychological factors such as stress influence the immune system and immune functioning. The term psychoneuroimmunology was first coined in 1981, when it appeared as the title of a book that reviewed available evidence for associations between the brain, endocrine system, and immune system (Zacharie, 2009). To a large extent, this field evolved from the discovery that there is a connection between the central nervous system and the immune system.
Some of the most compelling evidence for a connection between the brain and the immune system comes from studies in which researchers demonstrated that immune responses in animals could be classically conditioned (Everly & Lating, 2002). For example, Ader and Cohen (1975) paired flavored water (the conditioned stimulus) with the presentation of an immunosuppressive drug (the unconditioned stimulus), causing sickness (an unconditioned response). Not surprisingly, rats exposed to this pairing developed a conditioned aversion to the flavored water. However, the taste of the water itself later produced immunosuppression (a conditioned response), indicating that the immune system itself had been conditioned. Many subsequent studies over the years have further demonstrated that immune responses can be classically conditioned in both animals and humans (Ader & Cohen, 2001). Thus, if classical conditioning can alter immunity, other psychological factors should be capable of altering it as well.
Hundreds of studies involving tens of thousands of participants have tested many kinds of brief and chronic stressors and their effect on the immune system (e.g., public speaking, medical school examinations, unemployment, marital discord, divorce, death of spouse, burnout and job strain, caring for a relative with Alzheimer’s disease, and exposure to the harsh climate of Antarctica). It has been repeatedly demonstrated that many kinds of stressors are associated with poor or weakened immune functioning (Glaser & Kiecolt-Glaser, 2005; Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002; Segerstrom & Miller, 2004).
When evaluating these findings, it is important to remember that there is a tangible physiological connection between the brain and the immune system. For example, the sympathetic nervous system innervates immune organs such as the thymus, bone marrow, spleen, and even lymph nodes (Maier, Watkins, & Fleshner, 1994). Also, we noted earlier that stress hormones released during hypothalamic-pituitary-adrenal (HPA) axis activation can adversely impact immune function. One way they do this is by inhibiting the production of lymphocytes, white blood cells that circulate in the body’s fluids that are important in the immune response (Everly & Lating, 2002).
Some of the more dramatic examples demonstrating the link between stress and impaired immune function involve studies in which volunteers were exposed to viruses. The rationale behind this research is that because stress weakens the immune system, people with high stress levels should be more likely to develop an illness compared to those under little stress. In one memorable experiment using this method, researchers interviewed 276 healthy volunteers about recent stressful experiences (Cohen et al., 1998). Following the interview, these participants were given nasal drops containing the cold virus (in case you are wondering why anybody would ever want to participate in a study in which they are subjected to such treatment, the participants were paid $800 for their trouble). When examined later, participants who reported experiencing chronic stressors for more than one month—especially enduring difficulties involving work or relationships—were considerably more likely to have developed colds than were participants who reported no chronic stressors (Figure 1).
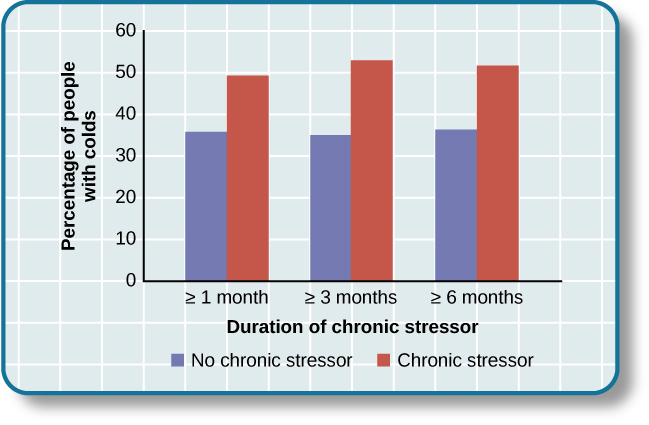
Figure 12. This graph shows the percentages of participants who developed colds (after receiving the cold virus) after reporting having experienced chronic stressors lasting at least one month, three months, and six months (adapted from Cohen et al., 1998).
In another study, older volunteers were given an influenza virus vaccination. Compared to controls, those who were caring for a spouse with Alzheimer’s disease (and thus were under chronic stress) showed poorer antibody response following the vaccination (Kiecolt-Glaser, Glaser, Gravenstein, Malarkey, & Sheridan, 1996).
Other studies have demonstrated that stress slows down wound healing by impairing immune responses important to wound repair (Glaser & Kiecolt-Glaser, 2005). In one study, for example, skin blisters were induced on the forearm. Subjects who reported higher levels of stress produced lower levels of immune proteins necessary for wound healing (Glaser et al., 1999). Stress, then, is not so much the sword that kills the knight, so to speak; rather, it’s the sword that breaks the knight’s shield, and your immune system is that shield.
Stress and Aging: A Tale of Telomeres
Have you ever wondered why people who are stressed often seem to have a haggard look about them? A pioneering study from 2004 suggests that the reason is because stress can actually accelerate the cell biology of aging.
Stress, it seems, can shorten telomeres, which are segments of DNA that protect the ends of chromosomes. Shortened telomeres can inhibit or block cell division, which includes growth and proliferation of new cells, thereby leading to more rapid aging (Sapolsky, 2004). In the study, researchers compared telomere lengths in the white blood cells in mothers of chronically ill children to those of mothers of healthy children (Epel et al., 2004). Mothers of chronically ill children would be expected to experience more stress than would mothers of healthy children. The longer a mother had spent caring for her ill child, the shorter her telomeres (the correlation between years of caregiving and telomere length was r = -.40). In addition, higher levels of perceived stress were negatively correlated with telomere size (r = -.31). These researchers also found that the average telomere length of the most stressed mothers, compared to the least stressed, was similar to what you would find in people who were 9–17 years older than they were on average.
Numerous other studies since have continued to find associations between stress and eroded telomeres (Blackburn & Epel, 2012). Some studies have even demonstrated that stress can begin to erode telomeres in childhood and perhaps even before children are born. For example, childhood exposure to violence (e.g., maternal domestic violence, bullying victimization, and physical maltreatment) was found in one study to accelerate telomere erosion from ages 5 to 10 (Shalev et al., 2013). Another study reported that young adults whose mothers had experienced severe stress during their pregnancy had shorter telomeres than did those whose mothers had stress-free and uneventful pregnancies (Entringer et al., 2011). Further, the corrosive effects of childhood stress on telomeres can extend into young adulthood. In an investigation of over 4,000 U.K. women ages 41–80, adverse experiences during childhood (e.g., physical abuse, being sent away from home, and parent divorce) were associated with shortened telomere length (Surtees et al., 2010), and telomere size decreased as the amount of experienced adversity increased (Figure 13).

Figure 13. Telomeres are shorter in adults who experienced more trauma as children (adapted from Blackburn & Epel, 2012).
Efforts to dissect the precise cellular and physiological mechanisms linking short telomeres to stress and disease are currently underway. For the time being, telomeres provide us with yet another reminder that stress, especially during early life, can be just as harmful to our health as smoking or fast food (Blackburn & Epel, 2012).
Try It
Cardiovascular Disorders
The cardiovascular system is composed of the heart and blood circulation system. For many years, disorders that involve the cardiovascular system—known as cardiovascular disorders—have been a major focal point in the study of psychophysiological disorders because of the cardiovascular system’s centrality in the stress response (Everly & Lating, 2002). Heart disease is one such condition. Each year, heart disease causes approximately one in three deaths in the United States, and it is the leading cause of death in the developed world (Centers for Disease Control and Prevention [CDC], 2011; Shapiro, 2005).
The symptoms of heart disease vary somewhat depending on the specific kind of heart disease one has, but they generally involve angina—chest pains or discomfort that occur when the heart does not receive enough blood (Office on Women’s Health, 2009). The pain often feels like the chest is being pressed or squeezed; burning sensations in the chest and shortness of breath are also commonly reported. Such pain and discomfort can spread to the arms, neck, jaws, stomach (as nausea), and back (American Heart Association [AHA], 2012a) (Figure 3).

Figure 14. Males and females often experience different symptoms of a heart attack.
A major risk factor for heart disease is hypertension, which is high blood pressure. Hypertension forces a person’s heart to pump harder, thus putting more physical strain on the heart. If left unchecked, hypertension can lead to a heart attack, stroke, or heart failure; it can also lead to kidney failure and blindness. Hypertension is a serious cardiovascular disorder, and it is sometimes called the silent killer because it has no symptoms—one who has high blood pressure may not even be aware of it (AHA, 2012b).
Many risk factors contributing to cardiovascular disorders have been identified. These risk factors include social determinants such as aging, income, education, and employment status, as well as behavioral risk factors that include unhealthy diet, tobacco use, physical inactivity, and excessive alcohol consumption; obesity and diabetes are additional risk factors (World Health Organization [WHO], 2013).
Over the past few decades, there has been much greater recognition and awareness of the importance of stress and other psychological factors in cardiovascular health (Nusair, Al-dadah, & Kumar, 2012). Indeed, exposure to stressors of many kinds has also been linked to cardiovascular problems; in the case of hypertension, some of these stressors include job strain (Trudel, Brisson, & Milot, 2010), natural disasters (Saito, Kim, Maekawa, Ikeda, & Yokoyama, 1997), marital conflict (Nealey-Moore, Smith, Uchino, Hawkins, & Olson-Cerny, 2007), and exposure to high traffic noise levels at one’s home (de Kluizenaar, Gansevoort, Miedema, & de Jong, 2007). Perceived discrimination appears to be associated with hypertension among African Americans (Sims et al., 2012). In addition, laboratory-based stress tasks, such as performing mental arithmetic under time pressure, immersing one’s hand into ice water (known as the cold pressor test), mirror tracing, and public speaking have all been shown to elevate blood pressure (Phillips, 2011).
Are you Type A or Type B?
Sometimes research ideas and theories emerge from seemingly trivial observations. In the 1950s, cardiologist Meyer Friedman was looking over his waiting room furniture, which consisted of upholstered chairs with armrests. Friedman decided to have these chairs reupholstered. When the man doing the reupholstering came to the office to do the work, he commented on how the chairs were worn in a unique manner—the front edges of the cushions were worn down, as were the front tips of the arm rests. It seemed like the cardiology patients were tapping or squeezing the front of the armrests, as well as literally sitting on the edge of their seats (Friedman & Rosenman, 1974). Were cardiology patients somehow different than other types of patients? If so, how?
After researching this matter, Friedman and his colleague, Ray Rosenman, came to understand that people who are prone to heart disease tend to think, feel, and act differently than those who are not. These individuals tend to be intensively driven workaholics who are preoccupied with deadlines and always seem to be in a rush. According to Friedman and Rosenman, these individuals exhibit Type A behavior pattern; those who are more relaxed and laid-back were characterized as Type B (Figure 4). In a sample of Type As and Type Bs, Friedman and Rosenman were startled to discover that heart disease was over seven times more frequent among the Type As than the Type Bs (Friedman & Rosenman, 1959).

Figure 15. (a) Type A individuals are characterized as intensely driven, (b) while Type B people are characterized as laid-back and relaxed. (credit a: modification of work by Greg Hernandez; credit b: modification of work by Elvert Barnes)
The major components of the Type A pattern include an aggressive and chronic struggle to achieve more and more in less and less time (Friedman & Rosenman, 1974). Specific characteristics of the Type A pattern include an excessive competitive drive, chronic sense of time urgency, impatience, and hostility toward others (particularly those who get in the person’s way).
An example of a person who exhibits Type A behavior pattern is Jeffrey. Even as a child, Jeffrey was intense and driven. He excelled at school, was captain of the swim team, and graduated with honors from an Ivy League college. Jeffrey never seems able to relax; he is always working on something, even on the weekends. However, Jeffrey always seems to feel as though there are not enough hours in the day to accomplish all he feels he should. He volunteers to take on extra tasks at work and often brings his work home with him; he often goes to bed angry late at night because he feels that he has not done enough. Jeffrey is quick tempered with his coworkers; he often becomes noticeably agitated when dealing with those coworkers he feels work too slowly or whose work does not meet his standards. He typically reacts with hostility when interrupted at work. He has experienced problems in his marriage over his lack of time spent with family. When caught in traffic during his commute to and from work, Jeffrey incessantly pounds on his horn and swears loudly at other drivers. When Jeffrey was 52, he suffered his first heart attack.
By the 1970s, a majority of practicing cardiologists believed that Type A behavior pattern was a significant risk factor for heart disease (Friedman, 1977). Indeed, a number of early longitudinal investigations demonstrated a link between Type A behavior pattern and later development of heart disease (Rosenman et al., 1975; Haynes, Feinleib, & Kannel, 1980).
Subsequent research examining the association between Type A and heart disease, however, failed to replicate these earlier findings (Glassman, 2007; Myrtek, 2001). Because Type A theory did not pan out as well as they had hoped, researchers shifted their attention toward determining if any of the specific elements of Type A predict heart disease.
Extensive research clearly suggests that the anger/hostility dimension of Type A behavior pattern may be one of the most important factors in the development of heart disease. This relationship was initially described in the Haynes et al. (1980) study mentioned above: Suppressed hostility was found to substantially elevate the risk of heart disease for both men and women. Also, one investigation followed over 1,000 male medical students from 32 to 48 years. At the beginning of the study, these men completed a questionnaire assessing how they react to pressure; some indicated that they respond with high levels of anger, whereas others indicated that they respond with less anger. Decades later, researchers found that those who earlier had indicated the highest levels of anger were over 6 times more likely than those who indicated less anger to have had a heart attack by age 55, and they were 3.5 times more likely to have experienced heart disease by the same age (Chang, Ford, Meoni, Wang, & Klag, 2002). From a health standpoint, it clearly does not pay to be an angry young person.
After reviewing and statistically summarizing 35 studies from 1983 to 2006, Chida and Steptoe (2009) concluded that the bulk of the evidence suggests that anger and hostility constitute serious long-term risk factors for adverse cardiovascular outcomes among both healthy individuals and those already suffering from heart disease. One reason angry and hostile moods might contribute to cardiovascular diseases is that such moods can create social strain, mainly in the form of antagonistic social encounters with others. This strain could then lay the foundation for disease-promoting cardiovascular responses among hostile individuals (Vella, Kamarck, Flory, & Manuck, 2012). In this transactional model, hostility and social strain form a cycle (Figure 5).

Figure 16. According to the transactional model of hostility for predicting social interactions (Vella et al., 2012), the thoughts and feelings of a hostile person promote antagonistic behavior toward others, which in turn reinforces complimentary reactions from others, thereby intensifying ones’ hostile disposition and intensifying the cyclical nature of this relationship.
For example, suppose Kaitlin has a hostile disposition; she has a cynical, distrustful attitude toward others and often thinks that other people are out to get her. She is very defensive around people, even those she has known for years, and she is always looking for signs that others are either disrespecting or belittling her. In the shower each morning before work, she often mentally rehearses what she would say to someone who said or did something that angered her, such as making a political statement that was counter to her own ideology. As Kaitlin goes through these mental rehearsals, she often grins and thinks about the retaliation on anyone who will irk her that day.
Socially, she is confrontational and tends to use a harsh tone with people, which often leads to very disagreeable and sometimes argumentative social interactions. As you might imagine, Kaitlin is not especially popular with others, including coworkers, neighbors, and even members of her own family. They either avoid her at all costs or snap back at her, which causes Kaitlin to become even more cynical and distrustful of others, making her disposition even more hostile. Kaitlin’s hostility—through her own doing—has created an antagonistic environment that cyclically causes her to become even more hostile and angry, thereby potentially setting the stage for cardiovascular problems.
In addition to anger and hostility, a number of other negative emotional states have been linked with heart disease, including negative affectivity and depression (Suls & Bunde, 2005). Negative affectivity is a tendency to experience distressed emotional states involving anger, contempt, disgust, guilt, fear, and nervousness (Watson, Clark, & Tellegen, 1988). It has been linked with the development of both hypertension and heart disease. For example, over 3,000 initially healthy participants in one study were tracked longitudinally, up to 22 years. Those with higher levels of negative affectivity at the time the study began were substantially more likely to develop and be treated for hypertension during the ensuing years than were those with lower levels of negative affectivity (Jonas & Lando, 2000). In addition, a study of over 10,000 middle-aged London-based civil servants who were followed an average of 12.5 years revealed that those who earlier had scored in the upper third on a test of negative affectivity were 32% more likely to have experienced heart disease, heart attack, or angina over a period of years than were those who scored in the lowest third (Nabi, Kivimaki, De Vogli, Marmot, & Singh-Manoux, 2008). Hence, negative affectivity appears to be a potentially vital risk factor for the development of cardiovascular disorders.
Coping with Stress
As you learned in the previous section, stress—especially if it is chronic—takes a toll on our bodies and can have enormously negative health implications. When we experience events in our lives that we appraise as stressful, it is essential that we use effective coping strategies to manage our stress. Coping refers to mental and behavioral efforts that we use to deal with problems relating to stress, including its presumed cause and the unpleasant feelings and emotions it produces.
Happiness is conceptualized as an enduring state of mind that consists of the capacity to experience pleasure in daily life, as well as the ability to engage one’s skills and talents to enrich one’s life and the lives of others. Although people around the world generally report that they are happy, there are differences in average happiness levels across nations. Although people have a tendency to overestimate the extent to which their happiness set points would change for the better or for the worse following certain life events, researchers have identified a number of factors that are consistently related to happiness. In recent years, positive psychology has emerged as an area of study seeking to identify and promote qualities that lead to greater happiness and fulfillment in our lives. These components include positive affect, optimism, and flow.
Coping Styles
Lazarus and Folkman (1984) distinguished two fundamental kinds of coping: problem-focused coping and emotion-focused coping. In problem-focused coping, one attempts to manage or alter the problem that is causing one to experience stress (i.e., the stressor). Problem-focused coping strategies are similar to strategies used in everyday problem-solving: they typically involve identifying the problem, considering possible solutions, weighing the costs and benefits of these solutions, and then selecting an alternative (Lazarus & Folkman, 1984). As an example, suppose Bradford receives a midterm notice that he is failing statistics class. If Bradford adopts a problem-focused coping approach to managing his stress, he would be proactive in trying to alleviate the source of the stress. He might contact his professor to discuss what must be done to raise his grade, he might also decide to set aside two hours daily to study statistics assignments, and he may seek tutoring assistance. A problem-focused approach to managing stress means we actively try to do things to address the problem.
Emotion-focused coping, in contrast, consists of efforts to change or reduce the negative emotions associated with stress. These efforts may include avoiding, minimizing, or distancing oneself from the problem, or positive comparisons with others (“I’m not as bad off as she is”), or seeking something positive in a negative event (“Now that I’ve been fired, I can sleep in for a few days”). In some cases, emotion-focused coping strategies involve reappraisal, whereby the stressor is construed differently (and somewhat self-deceptively) without changing its objective level of threat (Lazarus & Folkman, 1984). For example, a person sentenced to federal prison who thinks, “This will give me a great chance to network with others,” is using reappraisal. If Bradford adopted an emotion-focused approach to managing his midterm deficiency stress, he might watch a comedy movie, play video games, or spend hours on Twitter to take his mind off the situation. In a certain sense, emotion-focused coping can be thought of as treating the symptoms rather than the actual cause.
While many stressors elicit both kinds of coping strategies, problem-focused coping is more likely to occur when encountering stressors we perceive as controllable, while emotion-focused coping is more likely to predominate when faced with stressors that we believe we are powerless to change (Folkman & Lazarus, 1980). Clearly, emotion-focused coping is more effective in dealing with uncontrollable stressors. For example, if at midnight you are stressing over a 40-page paper due in the morning that you have not yet started, you are probably better off recognizing the hopelessness of the situation and doing something to take your mind off it; taking a problem-focused approach by trying to accomplish this task would only lead to frustration, anxiety, and even more stress.
Fortunately, most stressors we encounter can be modified and are, to varying degrees, controllable. A person who cannot stand her job can quit and look for work elsewhere; a middle-aged divorcee can find another potential partner; the freshman who fails an exam can study harder next time, and a breast lump does not necessarily mean that one is fated to die of breast cancer.
Try It
Defense Mechanisms
Freud believed that feelings of anxiety result from the ego’s inability to mediate the conflict between the id and superego. When this happens, Freud believed that the ego seeks to restore balance through various protective measures known as defense mechanisms (Figure 6). When certain events, feelings, or yearnings cause an individual anxiety, the individual wishes to reduce that anxiety. To do that, the individual’s unconscious mind uses ego defense mechanisms, unconscious protective behaviors that aim to reduce anxiety. The ego, usually conscious, resorts to unconscious strivings to protect the ego from being overwhelmed by anxiety. When we use defense mechanisms, we are unaware that we are using them. Further, they operate in various ways that distort reality. According to Freud, we all use ego defense mechanisms.
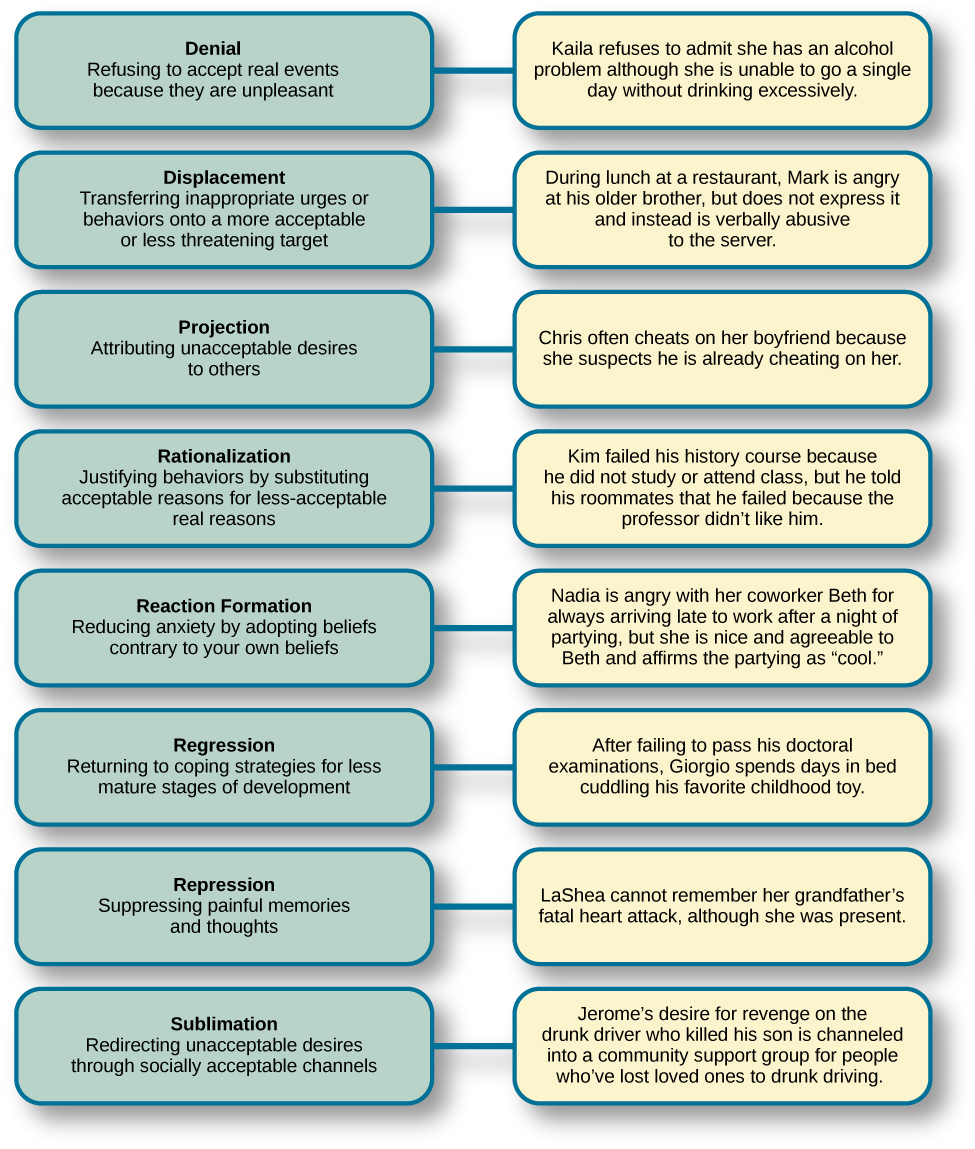
Figure 17. Defense mechanisms are unconscious protective behaviors that work to reduce anxiety.
While everyone uses defense mechanisms, Freud believed that overuse of them may be problematic. For example, let’s say Joe Smith is a high school football player. Deep down, Joe feels sexually attracted to males. His conscious belief is that being gay is immoral and that if he were gay, his family would disown him and he would be ostracized by his peers. Therefore, there is a conflict between his conscious beliefs (being gay is wrong and will result in being ostracized) and his unconscious urges (attraction to males). The idea that he might be gay causes Joe to have feelings of anxiety. How can he decrease his anxiety? Joe may find himself acting very “macho,” making gay jokes, and picking on a school peer who is gay. This way, Joe’s unconscious impulses are further submerged.
There are several different types of defense mechanisms. For instance, in repression, anxiety-causing memories from consciousness are blocked. As an analogy, let’s say your car is making a strange noise, but because you do not have the money to get it fixed, you just turn up the radio so that you no longer hear the strange noise. Eventually you forget about it. Similarly, in the human psyche, if a memory is too overwhelming to deal with, it might be repressed and thus removed from conscious awareness (Freud, 1920). This repressed memory might cause symptoms in other areas.
Another defense mechanism is reaction formation, in which someone expresses feelings, thoughts, and behaviors opposite to their inclinations. In the above example, Joe made fun of a homosexual peer while himself being attracted to males. In regression, an individual acts much younger than their age. For example, a four-year-old child who resents the arrival of a newborn sibling may act like a baby and revert to drinking out of a bottle. In projection, a person refuses to acknowledge her own unconscious feelings and instead sees those feelings in someone else. Other defense mechanisms include rationalization, displacement, and sublimation.
Try It
Control and Stress
The desire and ability to predict events, make decisions, and affect outcomes—that is, to enact control in our lives—is a basic tenet of human behavior (Everly & Lating, 2002). Albert Bandura (1997) stated that “the intensity and chronicity of human stress is governed largely by perceived control over the demands of one’s life” (p. 262). As cogently described in his statement, our reaction to potential stressors depends to a large extent on how much control we feel we have over such things. Perceived control is our beliefs about our personal capacity to exert influence over and shape outcomes, and it has major implications for our health and happiness (Infurna & Gerstorf, 2014). Extensive research has demonstrated that perceptions of personal control are associated with a variety of favorable outcomes, such as better physical and mental health and greater psychological well-being (Diehl & Hay, 2010). Greater personal control is also associated with lower reactivity to stressors in daily life. For example, researchers in one investigation found that higher levels of perceived control at one point in time were later associated with lower emotional and physical reactivity to interpersonal stressors (Neupert, Almeida, & Charles, 2007). Further, a daily diary study with 34 older widows found that their stress and anxiety levels were significantly reduced on days during which the widows felt greater perceived control (Ong, Bergeman, & Bisconti, 2005).
The link between perceived control and health may provide an explanation for the frequently observed relationship between social class and health outcomes (Kraus, Piff, Mendoza-Denton, Rheinschmidt, & Keltner, 2012). In general, research has found that more affluent individuals experience better health mainly because they tend to believe that they can personally control and manage their reactions to life’s stressors (Johnson & Krueger, 2006). Perhaps buoyed by the perceived level of control, individuals of higher social class may be prone to overestimating the degree of influence they have over particular outcomes. For example, those of higher social class tend to believe that their votes have greater sway on election outcomes than do those of lower social class, which may explain higher rates of voting in more affluent communities (Krosnick, 1990). Other research has found that a sense of perceived control can protect less affluent individuals from poorer health, depression, and reduced life-satisfaction—all of which tend to accompany lower social standing (Lachman & Weaver, 1998).
Taken together, findings from these and many other studies clearly suggest that perceptions of control and coping abilities are important in managing and coping with the stressors we encounter throughout life.
Try It
Social Support
The need to form and maintain strong, stable relationships with others is a powerful, pervasive, and fundamental human motive (Baumeister & Leary, 1995). Building strong interpersonal relationships with others helps us establish a network of close, caring individuals who can provide social support in times of distress, sorrow, and fear. Social support can be thought of as the soothing impact of friends, family, and acquaintances (Baron & Kerr, 2003). Social support can take many forms, including advice, guidance, encouragement, acceptance, emotional comfort, and tangible assistance (such as financial help). Thus, other people can be very comforting to us when we are faced with a wide range of life stressors, and they can be extremely helpful in our efforts to manage these challenges. Even in nonhuman animals, species mates can offer social support during times of stress. For example, elephants seem to be able to sense when other elephants are stressed and will often comfort them with physical contact—such as a trunk touch—or an empathetic vocal response (Krumboltz, 2014).
Scientific interest in the importance of social support first emerged in the 1970s when health researchers developed an interest in the health consequences of being socially integrated (Stroebe & Stroebe, 1996). Interest was further fueled by longitudinal studies showing that social connectedness reduced mortality. In one classic study, nearly 7,000 Alameda County, California, residents were followed over 9 years. Those who had previously indicated that they lacked social and community ties were more likely to die during the follow-up period than those with more extensive social networks. Compared to those with the most social contacts, isolated men and women were, respectively, 2.3 and 2.8 times more likely to die. These trends persisted even after controlling for a variety of health-related variables, such as smoking, alcohol consumption, self-reported health at the beginning of the study, and physical activity (Berkman & Syme, 1979).
Since the time of that study, social support has emerged as one of the well-documented psychosocial factors affecting health outcomes (Uchino, 2009). A statistical review of 148 studies conducted between 1982 and 2007 involving over 300,000 participants concluded that individuals with stronger social relationships have a 50% greater likelihood of survival compared to those with weak or insufficient social relationships (Holt-Lunstad, Smith, & Layton, 2010). According to the researchers, the magnitude of the effect of social support observed in this study is comparable with quitting smoking and exceeded many well-known risk factors for mortality, such as obesity and physical inactivity.

Figure 18. Close relationships with others, whether (a) a group of friends or (b) a family circle, provide more than happiness and fulfillment—they can help foster good health. (credit a: modification of work by Nattachai Noogure; credit b: modification of work by Christian Haugen)
A number of large-scale studies have found that individuals with low levels of social support are at greater risk of mortality, especially from cardiovascular disorders (Brummett et al., 2001). Further, higher levels of social supported have been linked to better survival rates following breast cancer (Falagas et al., 2007) and infectious diseases, especially HIV infection (Lee & Rotheram-Borus, 2001). In fact, a person with high levels of social support is less likely to contract a common cold. In one study, 334 participants completed questionnaires assessing their sociability; these individuals were subsequently exposed to a virus that causes a common cold and monitored for several weeks to see who became ill. Results showed that increased sociability was linearly associated with a decreased probability of developing a cold (Cohen, Doyle, Turner, Alper, & Skoner, 2003).
For many of us, friends are a vital source of social support. But what if you found yourself in a situation in which you lacked friends or companions? For example, suppose a popular high school student attends a far-away college, does not know anyone, and has trouble making friends and meaningful connections with others during the first semester. What can be done? If real life social support is lacking, access to distant friends via social media may help compensate. In a study of college freshmen, those with few face-to-face friends on campus but who communicated electronically with distant friends were less distressed that those who did not (Raney & Troop-Gordon, 2012). Also, for some people, our families—especially our parents—are a major source of social support.
Social support appears to work by boosting the immune system, especially among people who are experiencing stress (Uchino, Vaughn, Carlisle, & Birmingham, 2012). In a pioneering study, spouses of cancer patients who reported high levels of social support showed indications of better immune functioning on two out of three immune functioning measures, compared to spouses who were below the median on reported social support (Baron, Cutrona, Hicklin, Russell, & Lubaroff, 1990). Studies of other populations have produced similar results, including those of spousal caregivers of dementia sufferers, medical students, elderly adults, and cancer patients (Cohen & Herbert, 1996; Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002).
In addition, social support has been shown to reduce blood pressure for people performing stressful tasks, such as giving a speech or performing mental arithmetic (Lepore, 1998). In these kinds of studies, participants are usually asked to perform a stressful task either alone, with a stranger present (who may be either supportive or unsupportive), or with a friend present. Those tested with a friend present generally exhibit lower blood pressure than those tested alone or with a stranger (Fontana, Diegnan, Villeneuve, & Lepore, 1999). In one study, 112 female participants who performed stressful mental arithmetic exhibited lower blood pressure when they received support from a friend rather than a stranger, but only if the friend was a male (Phillips, Gallagher, & Carroll, 2009). Although these findings are somewhat difficult to interpret, the authors mention that it is possible that females feel less supported and more evaluated by other females, particularly females whose opinions they value.
Taken together, the findings above suggest one of the reasons social support is connected to favorable health outcomes is because it has several beneficial physiological effects in stressful situations. However, it is also important to consider the possibility that social support may lead to better health behaviors, such as a healthy diet, exercising, smoking cessation, and cooperation with medical regimens (Uchino, 2009).
Try It
Stress Reduction Techniques

Figure 19. Stress reduction techniques may include (a) exercise, (b) meditation and relaxation, or (c) biofeedback. (credit a: modification of work by “UNE Photos”/Flickr; credit b: modification of work by Caleb Roenigk; credit c: modification of work by Dr. Carmen Russoniello)
One reason exercise may be beneficial is because it might buffer some of the deleterious physiological mechanisms of stress. One study found rats that exercised for six weeks showed a decrease in hypothalamic-pituitary-adrenal responsiveness to mild stressors (Campeau et al., 2010). In high-stress humans, exercise has been shown to prevent telomere shortening, which may explain the common observation of a youthful appearance among those who exercise regularly (Puterman et al., 2010). Further, exercise in later adulthood appears to minimize the detrimental effects of stress on the hippocampus and memory (Head, Singh, & Bugg, 2012). Among cancer survivors, exercise has been shown to reduce anxiety (Speck, Courneya, Masse, Duval, & Schmitz, 2010) and depressive symptoms (Craft, VanIterson, Helenowski, Rademaker, & Courneya, 2012). Clearly, exercise is a highly effective tool for regulating stress.
In the 1970s, Herbert Benson, a cardiologist, developed a stress reduction method called the relaxation response technique (Greenberg, 2006). The relaxation response technique combines relaxation with transcendental meditation, and consists of four components (Stein, 2001): sitting upright on a comfortable chair with feet on the ground and body in a relaxed position, a quiet environment with eyes closed, repeating a word or a phrase—a mantra—to oneself, such as “alert mind, calm body,” passively allowing the mind to focus on pleasant thoughts, such as nature or the warmth of your blood nourishing your body.
The relaxation response approach is conceptualized as a general approach to stress reduction that reduces sympathetic arousal, and it has been used effectively to treat people with high blood pressure (Benson & Proctor, 1994).
Another technique to combat stress, biofeedback, was developed by Gary Schwartz at Harvard University in the early 1970s. Biofeedback is a technique that uses electronic equipment to accurately measure a person’s neuromuscular and autonomic activity—feedback is provided in the form of visual or auditory signals. The main assumption of this approach is that providing somebody biofeedback will enable the individual to develop strategies that help gain some level of voluntary control over what are normally involuntary bodily processes (Schwartz & Schwartz, 1995). A number of different bodily measures have been used in biofeedback research, including facial muscle movement, brain activity, and skin temperature, and it has been applied successfully with individuals experiencing tension headaches, high blood pressure, asthma, and phobias (Stein, 2001).

