Now that you know the basics of what vitamins are, let’s talk about the Fat Soluble Vitamins (FSV’s) specifically. There are only four FSV’s: Vitamin A, Vitamin D, Vitamin E and Vitamin K. What makes them “fat soluble” is the fact that they dissolve in fats and oils but they won’t dissolve in water. If you’ve ever seen a vitamin E capsule, you already know that inside the capsule is an oily substance containing vitamin E. The Fat soluble vitamins are present in many foods but they are especially high in foods like nuts and seeds that contain a high concentration of fats and oils. Though we will discuss each fat soluble vitamin separately, please keep in mind that in whole foods there are a variety of vitamins and minerals and other nutrients all working together. This is thought to be the reason that whole foods do such good things for the body whereas taking individual supplements doesn’t usually benefit health and sometimes can be harmful. Many scientists and doctors (myself included) believe that it is the harmony of the nutrients coming in together that benefits our health and when we isolate an individual nutrient it cannot give the same benefits.
7.2A: Vitamin A
- Preformed vitamin A is found in animal products such as meat, fish, poultry and dairy foods.
- Pro-vitamin A is found in plant-based foods such as fruits and vegetables. The most common type of pro-vitamin A is beta-carotene. Pro-vitamin A must be converted into active vitamin A by the body.
Vitamin A is also available in dietary supplements. It most often comes in the form of retinyl acetate or retinyl palmitate (preformed vitamin A), beta-carotene (pro-vitamin A) or a combination of preformed and pro-vitamin A.
Function of Vitamin A
Vitamin A helps form and maintain healthy skin, teeth, skeletal and soft tissue, mucus membranes, and skin. It is also known as retinol because it produces the pigments in the retina of the eye. Vitamin A promotes good vision, especially in low light. It may also be needed for reproduction and breast-feeding. Retinol is an active form of vitamin A. It is found in animal liver, whole milk, and some fortified foods. Carotenoids are dark-colored dyes (pigments) found in plant foods that can turn into a form of vitamin A. There are more than 500 known carotenoids. One such carotenoid is beta-carotene.
- Beta-carotene is an antioxidant. Antioxidants protect cells from damage caused by substances called free radicals. Free radicals are believed to contribute to certain chronic diseases and play a role in the aging processes.
- Diets containing food sources of carotenoids such as beta-carotene have been shown to reduce the risk for cancer.
- Beta-carotene supplements (isolated Beta-carotene in concentrated form) do not seem to reduce cancer risk.
Video 7.2A.1: This video connects health-conscious individuals with important news and information in the fast-paced world of health. From recalls and outbreaks to diet, nutrition and fitness we cover everything you need to know about health, every day.
Food Sources of Vitamin A
Vitamin A comes from animal sources, such as eggs, meat, fortified milk, cheese, cream, liver, kidney, cod, and halibut fish oil. However, all of these sources, except for skim milk that has been fortified with Vitamin A, are high in saturated fat and cholesterol. Some good sources of vitamin A are:
- Eggs (preformed vitamin A)
- Milk and other dairy products (preformed vitamin A)
- Orange and yellow vegetables and fruits (pro-vitamin A)
- Other sources of beta-carotene such as broccoli, spinach, and most dark green, leafy vegetables (pro-vitamin A)
The more intense the color of a fruit or vegetable, the higher the beta-carotene content. Vegetable sources of beta-carotene are cholesterol-free.
Side Effects of too much or too little Vitamin A
If you do not get enough vitamin A, you are at increased risk for eye problems. These include reversible night blindness and then non-reversible corneal damage known as xeropthalmia. Lack of vitamin A can lead to hyperkeratosis or dry, scaly skin. If you get too much vitamin A, you can become sick. Large doses of vitamin A can also cause birth defects.

Acute vitamin A poisoning most often occurs when an adult takes several hundred thousand IUs of vitamin A. Symptoms of chronic vitamin A poisoning may occur in adults who regularly take more than 25,000 IU a day. Babies and children are more sensitive to vitamin A, and can become sick after taking smaller doses of vitamin A or vitamin A-containing products such as retinol (found in skin creams). Large amounts of beta-carotene do not cause harm. However, high levels of beta-carotene can turn the skin yellow or orange. The skin color will return to normal once you reduce your intake of beta-carotene.
Recommendations for Vitamin A
The best way to get the daily requirement of essential vitamins is to eat a wide variety of fruits, vegetables, fortified dairy foods, legumes (dried beans), lentils, and whole grains.
The Food and Nutrition Board of the Institute of Medicine — Dietary Reference Intakes (DRIs) Recommended Intakes for Individuals of Vitamin A:
Infants (average intake)
- 0 to 6 months: 400 micrograms per day (mcg/day)
- 7 to 12 months: 500 mcg/day
The Recommended Dietary Allowance (RDA) for vitamins is how much of each vitamin most people should get each day. The RDA for vitamins may be used as goals for each person.
Children (RDA)
- 1 to 3 years: 300 mcg/day
- 4 to 8 years: 400 mcg/day
- 9 to 13 years: 600 mcg/day
Adolescents and Adults (RDA)
- Males age 14 and older: 900 mcg/day
- Females age 14 and older: 700 mcg/day (770 during pregnancy and 1,300 mcg during lactation)
How much of each vitamin you need depends on your age and gender. Other factors, such as pregnancy and your health, are also important. Ask your health care provider what dose is best for you.
7.2B: Vitamin D
DEFICIENCY: RICKETS
A diet deficient in vitamin D in conjunction with inadequate sun exposure causes osteomalacia (or rickets when it occurs in children), which is a softening of the bones. In the developed world, this is a rare disease. However, vitamin D deficiency has become a worldwide problem in the elderly and remains common in children and adults. Low blood calcifediol (25-hydroxy-vitamin D) can result from avoiding the sun. Deficiency results in impaired bone mineralization and bone damage which leads to bone-softening diseases, including rickets and osteomalacia.
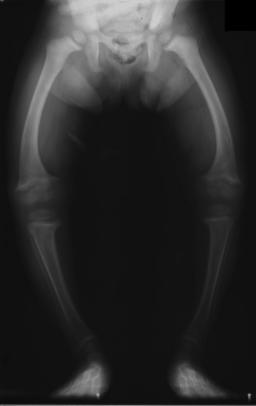
Legs in a 2 year old child with rickets. Image used with permission (CC BY-SA 1.0; Michael L. Richardson, M.D.).
Rickets, a childhood disease, is characterized by impeded growth and soft, weak, deformed long bones that bend and bow under their weight as children start to walk. This condition is characterized by bow legs,] which can be caused by calcium or phosphorus deficiency, as well as a lack of vitamin D; today, it is largely found in low-income countries in Africa, Asia, or the Middle East and in those with genetic disorders such as pseudovitamin D deficiency rickets. Maternal vitamin D deficiency may cause overt bone disease from before birth and impairment of bone quality after birth. Nutritional rickets exists in countries with intense year-round sunlight such as Nigeria and can occur without vitamin D deficiency.
Vitamin D deficiency remains the main cause of rickets among young infants in most countries, because breast milk is low in vitamin D and social customs and climatic conditions can prevent adequate sun exposure. In sunny countries such as Nigeria, South Africa, and Bangladesh, where the disease occurs among older toddlers and children, it has been attributed to low dietary calcium intakes, which are characteristic of cereal-based diets with limited access to dairy products.
Synthesis in the Skin
Vitamin D3 is produced photochemically from 7-dehydrocholesterol in the skin of most vertebrate animals, including humans. The precursor of vitamin D3, 7-dehydrocholesterol is produced in relatively large quantities. 7-Dehydrocholesterol reacts with UVB light at wavelengths between 270 and 300 nm, with peak synthesis occurring between 295 and 297 nm. These wavelengths are present in sunlight, as well as in the light emitted by the UV lamps in tanning beds (which produce ultraviolet primarily in the UVA spectrum, but typically produce 4% to 10% of the total UV emissions as UVB). Exposure to light through windows is insufficient because glass almost completely blocks UVB light.
Adequate amounts of vitamin D can be produced with moderate sun exposure to the face, arms and legs, averaging 5–30 minutes twice per week, or approximately 25% of the time for minimal sunburn. The darker the skin, and the weaker the sunlight, the more minutes of exposure are needed. Vitamin D overdose is impossible from UV exposure; the skin reaches an equilibrium where the vitamin degrades as fast as it is created.
Dietary Reference Intakes (USA)
Accordingly, the Dietary Reference Intake for vitamin D assumes no synthesis occurs and all of a person’s vitamin D is from food intake. As vitamin D is synthesized in adequate amounts by most mammals exposed to sunlight, it is not strictly a vitamin, and may be considered a hormone as its synthesis and activity occur in different locations. Vitamin D has a significant role in calcium homeostasis and metabolism. Its discovery was due to effort to find the dietary substance lacking in rickets.
Different institutions propose different recommendations concerning daily amounts of the vitamin.The recommended daily intake of vitamin D may not be sufficient if sunlight exposure is limited. According to the United States Institute of Medicine, the recommended dietary allowances (RDA) of vitamin D are (Conversion : 1 µg = 40 IU and 0.025 µg = 1 IU) :
| Age group | RDA (IU/day) |
|---|---|
| Infants 0–6 months | 400* |
| Infants 6–12 months | 400* |
| 1–70 years | 600 (15 μg/day) |
| 71+ years | 800 (20 μg/day) |
| Pregnant/Lactating | 600 (15 μg/day) |
- Asterisk for infants indicates adequate intake (AI) for infants, as an RDA has yet to be established for infants.
For U.S. food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of Daily Value (%DV). For vitamin D labeling purposes 100% of the Daily Value was 400 IU (10 μg), but as of May 2016 it has been revised to 800 IU (20 μg). A table of the pre-change adult Daily Values is provided at Reference Daily Intake. Food and supplement companies have until July 28, 2018 to comply with the change.
7.2C: Vitamin E
Vitamin E refers to a group of compounds that include both tocopherols and tocotrienols. Of the many different forms of vitamin E, γ-tocopherol is the most common form found in the North American diet. γ-Tocopherol can be found in corn oil, soybean oil, margarine, and dressings. α-tocopherol, the most biologically active form of vitamin E, is the second-most common form of vitamin E in the diet. This variant can be found most abundantly in wheat germ oil, sunflower, and safflower oils. As a fat-soluble antioxidant, it interrupts the propagation of reactive oxygen species that spread through biological membranes or through a fat when its lipid content undergoes oxidation by reacting with more-reactive lipid radicals to form more stable products. Regular consumption of more than 1,000 mg (1,500 IU) of tocopherols per day may be expected to cause hypervitaminosis E, with an associated risk of vitamin K deficiency and consequently of bleeding problems.

Sample of α-tocopherol, one of the various forms of vitamin E
Functions
Vitamin E has many biological functions, including its role as a fat-soluble antioxidant.
- As an antioxidant, vitamin E acts as a peroxyl radical scavenger, disabling the production of damaging free radicals in tissues, by reacting with them to form a tocopheryl radical, which will then be reduced by a hydrogen donor (such as vitamin C) and thus return to its reduced state. As it is fat-soluble, it is incorporated into cell membranes, which protects them from oxidative damage. Vitamin E has also found use as a commercial antioxidant in ultra high molecular weight polyethylene (UHMWPE) used in hip and knee implants by resisting oxidation.
- As an enzymatic activity regulator, for instance, protein kinase C (PKC), which plays a role in smooth muscle growth, can be inhibited by α-tocopherol. α-Tocopherol has a stimulatory effect on the dephosphorylation enzyme, protein phosphatase 2A, which in turn, cleaves phosphate groups from PKC, leading to its deactivation, bringing the smooth muscle growth to a halt.
- Vitamin E also has an effect on gene expression. Macrophages rich in cholesterol are found in atherosclerotic tissue. Scavenger receptor CD36 is a class B scavenger receptor found to be up-regulated by oxidized low density lipoprotein (LDL) and binds it. Treatment with α-tocopherol was found to downregulate the expression of the CD36 scavenger receptor gene and the scavenger receptor class A (SR-A) and modulates expression of the connective tissue growth factor (CTGF). The CTGF gene, when expressed, is responsible for the repair of wounds and regeneration of the extracellular tissue lost or damaged during atherosclerosis.
- Vitamin E also plays a role in eye and neurological functions, and inhibition of platelet coagulation.
- Vitamin E also protects lipids and prevents the oxidation of polyunsaturated fatty acids.
Although most vitamin E supplementation studies used α-tocopherol individually, this design of studying only one isoform of vitamin E may introduce errors in interpreting overall vitamin E effects; for example, using only α-tocopherol in studies of inflammation can reduce serum γ- and δ-tocopherol concentrations. Moreover, a 2013 review involving single long-term supplementation with α-tocopherol showed that many clinical studies revealed an inverse relationship between supplementation and cardiovascular disease risk or mortality, but other studies showed no effect.
Deficiency
Vitamin E deficiency can cause:
- spinocerebellar ataxia
- myopathies
- peripheral neuropathy
- ataxia
- skeletal myopathy
- retinopathy
- impairment of the immune response
- red blood cell destruction
SUPPLEMENTATION
Vitamin E supplementation has not been shown to have significant benefit for people who are healthy, and appears to be harmful. It does not improve blood sugar control in an unselected group of people with diabetes mellitus or decrease the risk of stroke. Daily supplementation of vitamin E does not decrease the risk of prostate cancer, and may increase it. Studies on its role in age-related macular degeneration are ongoing, though if it is of a combination of dietary antioxidants used to treat the condition it may increase the risk. Routine supplementation with vitamin E during pregnancy has been shown to offer no benefit to the mother or the child. Vitamin E has been reported to cause more side effects, such as abdominal pain in pregnant women, and also the increased risk of having early rupture of membranes at term.
Vitamin E, along with β-carotene and vitamin C, has no protective effect on reducing the risk of cataract, cataract extraction, progression of cataract, and slowing the loss of visual acuity.
Toxicity
The LD50, or the toxic dose required to kill 50% of group of rats and mice, respectively is 4000 mg of VitaminE E/kg of rat and 4000 mg of Vitamin E/kg of mouse. Comparatively speaking, and at lethal doses, Vitamin E is less toxic than table salt and acetaminophen and it is more toxic than ethanol and Vitamin C. Vitamin E can act as an anticoagulant, increasing the risk of bleeding problems. As a result, many agencies have set a tolerable upper intake levels (UL) at 1,000 mg (1,500 IU) per day. In combination with certain other drugs such as aspirin, hypervitaminosis E can be life-threatening. Hypervitaminosis E may also counteract vitamin K, leading to a vitamin K deficiency.
Dietary Reference Intake
The Food and Nutrition Board (FNB) of the U.S. Institute of Medicine updated Estimated Average Requirements (EARs) and Recommended Dietary Allowances (RDAs) for vitamin E in 2000. The current EAR for vitamin E for women and men ages 14 and up is 12 mg/day. The RDA is 15 mg/day. RDAs are higher than EARs so as to identify amounts that will cover people with higher than average requirements. RDA for pregnancy equals 15 mg/day. RDA for lactation equals 19 mg/day. For infants up to 12 months the Adequate Intake (AI) is 4–5 mg/day and for children ages 1–13 years the RDA increases with age from 6 to 11 mg/day. The FNB also sets Tolerable Upper Intake Levels (ULs) for vitamins and minerals when evidence is sufficient. In the case of vitamin E the UL is 1,000 mg/day.
For U.S. food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of Daily Value (%DV). For vitamin E labeling purposes 100% of the Daily Value was 30 mg, but as of May 2016 it has been revised to 15 mg. A table of the pre-change adult Daily Values is provided at Reference Daily Intake. Food and supplement companies have until July 28, 2018 to comply with the change.
VITAMIN E AND ATHEROSCLEROSIS
Atherosclerosis is a disease condition that refers to the buildup of plaque, which is a substance containing lipid and cholesterol (mainly the low-density lipoprotein or LDL cholesterol) on the inner layer of the arterial lumen. With the existing plaque, instead of being smooth and elastic, the layers become thickened and irregular and the lumen of the artery become narrower. This vessel-narrowing effect lead to a reduction of blood circulation and can lead to or worsen the condition of hypertension.
There are currently multiple theories explaining factors causing and affecting the cholesterol plaque build up within arteries with the most popular theory indicating that the rate of build up is affected by the oxidation of the LDL cholesterol. LDL cholesterol is one of the five major groups of lipoproteins with one of the physiological roles being lipid transportation. A typical LDL particle contain 2,700 fatty acid molecules and half of them are poly-unsaturated fatty acids, which are very oxidation sensitive. Once the oxidation of LDL occur, it will start a series of undesirable effects starting from the increase production of inflammatory cytokines by stimulating the endothelial cells and monocytes, followed by increased production of tissue factors, production of macrophages and monocytes, which eventually lead to the formation of foam cells and accelerated development of atherosclerosis. With the presence of adequate concentration of vitamin E, which is a very potent fat-soluble antioxidant, it can inhibit the oxidation of LDL, and this inhibition contributes protection against the development of atherosclerosis and can stabilize the existing plaque.
According to one meta-analysis, nine cohort studies showed that high intake of tocopherol was associated with a lower risk of cardiovascular diseases compared with lower intake. In this study, higher dietary, supplementation and combined vitamin E intake was also associated with lower disease incidents. In 1993, a study of 39,919 male health professionals aged 40 to 75 showed that consumption of more than 60 IU of vitamin E (any form) per day was associated with a lower incidence of coronary heart disease compared with less than 7.5 IU/day intake. This study also showed an inverse association between vitamin E supplementation and the incidence of heart disease.
A 2015 systematic review of clinical trials concluded that vitamin E supplementation alone improved endothelial function as determined by measurements of forearm blood flow, but when combined with vitamin C supplementation, it did not. A meta-analysis of clinical trials showed no significant association between vitamin E supplementation and cardiovascular mortality.
7.2D: Vitamin K
Vitamin K (Figure 1) is a group of structurally similar, fat-soluble vitamins the human body requires for complete synthesis of certain proteins that are needed for blood coagulation (blood clotting) and which the body also needs for controlling the binding of calcium in bones and other tissues. The vitamin K-related modification of the proteins allows them to bind calcium ions, which they cannot do otherwise.
In menaquinone, the side chain is composed of a varying number of isoprenoid residues. The most common number of these residues is four, since animal enzymes normally produce menaquinone-4 from plant phylloquinone. The three synthetic forms of vitamin K are vitamins K3 (menadione), K4, and K5, which are used in many areas, including the pet food industry (vitamin K3) and to inhibit fungal growth (vitamin K5).

Figure 1: (left) Vitamin K1 (phylloquinone) – both forms of the vitamin contain a functional naphthoquinone ring and an aliphatic side chain. Phylloquinone has a phytyl side chain.

Vitamin K2 (menaquinone).
The MK-4 form of vitamin K2 is produced by conversion of vitamin K1 in the testes, pancreas, and arterial walls. While major questions still surround the biochemical pathway for this transformation, the conversion is not dependent on gut bacteria, as it occurs in germ-free rats and in parenterally-administered K1in rats. In fact, tissues that accumulate high amounts of MK-4 have a remarkable capacity to convert up to 90% of the available K1 into MK-4. There is evidence that the conversion proceeds by removal of the phytyl tail of K1 to produce menadione as an intermediate, which is then condensed with an activated geranylgeranyl moiety (see also prenylation) to produce vitamin K2 in the MK-4 (menatetrione) form.
HEALTH EFFECTS OF VITAMIN K
Without vitamin K, blood coagulation is seriously impaired, and uncontrolled bleeding occurs. Preliminary clinical research indicates that deficiency of vitamin K may weaken bones, potentially leading to osteoporosis, and may promote calcification of arteries and other soft tissues. Our main sources of vitamin K are from leafy green vegetables and from the production by bacteria in our large intestine.
- Osteoporosis: A review of 2014 concluded that there is positive evidence that monotherapy using MK-4, one of the forms of Vitamin K2, reduces fracture incidence in post-menopausal women with osteoporosis, and suggested further research on the combined use of MK-4 with bisphosphonates. In contrast, an earlier review article of 2013 concluded that there is no good evidence that vitamin K supplementation helps prevent osteoporosis or fractures in postmenopausal women. A Cochrane systematic review of 2006 suggested that supplementation with Vitamin K1 and with MK4 reduces bone loss; in particular, a strong effect of MK-4 on incident fractures among Japanese patients was emphasized. A review article of 2016 suggested to consider, as one of several measures for bone health, increasing the intake of foods rich in vitamins K1 and K2.
- Cardiovascular health: Adequate intake of vitamin K is associated with the inhibition of arterial calcification and stiffening, but there have been few interventional studies and no good evidence that vitamin K supplementation is of any benefit in the primary prevention of cardiovascular disease. One 10-year population study, the Rotterdam Study, did show a clear and significant inverse relationship between the highest intake levels of menaquinone (mainly MK-4 from eggs and meat, and MK-8 and MK-9 from cheese) and cardiovascular disease and all-cause mortality in older men and women.
- Cancer: Vitamin K has been promoted in supplement form with claims it can slow tumor growth; there is however no good medical evidence that supports such claims.
- Coumarin poisoning: Vitamin K is part of the suggested treatment regime for poisoning by rodenticide (coumarin poisoning).
Although allergic reaction from supplementation is possible, no known toxicity is associated with high doses of the phylloquinone (vitamin K1) or menaquinone (vitamin K2) forms of vitamin K, so no tolerable upper intake level (UL) has been set. Blood clotting (coagulation) studies in humans using 45 mg per day of vitamin K2 (as MK-4) and even up to 135 mg per day (45 mg three times daily) of K2 (as MK-4), showed no increase in blood clot risk. Even doses in rats as high as 250 mg/kg, body weight did not alter the tendency for blood-clot formation to occur. Unlike the safe natural forms of vitamin K1 and vitamin K2 and their various isomers, a synthetic form of vitamin K, vitamin K3 (menadione), is demonstrably toxic at high levels. The U.S. FDA has banned this form from over-the-counter sale in the United States because large doses have been shown to cause allergic reactions, hemolytic anemia, and cytotoxicity in liver cells.
Phylloquinone (K1) or menaquinone (K2) are capable of reversing the anticoagulant activity of the anticoagulant warfarin (tradename Coumadin). Warfarin works by blocking recycling of vitamin K, so that the body and tissues have lower levels of active vitamin K, and thus a deficiency of vitamin K. Supplemental vitamin K (for which oral dosing is often more active than injectable dosing in human adults) reverses the vitamin K deficiency caused by warfarin, and therefore reduces the intended anticoagulant action of warfarin and related drugs. Sometimes small amounts of vitamin K are given orally to patients taking warfarin so that the action of the drug is more predictable. The proper anticoagulant action of the drug is a function of vitamin K intake and drug dose, and due to differing absorption must be individualized for each patient. The action of warfarin and vitamin K both require two to five days after dosing to have maximum effect, and neither warfarin or vitamin K shows much effect in the first 24 hours after they are given.
Absorption and Dietary Need
Previous theory held that dietary deficiency is extremely rare unless the small intestine was heavily damaged, resulting in malabsorption of the molecule. Another at-risk group for deficiency were those subject to decreased production of K2 by normal intestinal microbiota, as seen in broad spectrum antibiotic use. Taking broad-spectrum antibiotics can reduce vitamin K production in the gut by nearly 74% in people compared with those not taking these antibiotics. Diets low in vitamin K also decrease the body’s vitamin K concentration. Those with chronic kidney disease are at risk for vitamin K deficiency, as well as vitamin D deficiency, and particularly those with the apoE4 genotype. Additionally, in the elderly there is a reduction in vitamin K2 production. Like other lipid-soluble vitamins (A, D and E), vitamin K is stored in the fatty tissue of the human body.
The National Academy of Medicine (NAM) updated an estimate of what constitutes an Adequate Intake (AI) for vitamin K in 2001. The NAM does not distinguish between K1 and K2 – both are counted as vitamin K. At that time there was not sufficient evidence to set the more rigorous Estimated Average Requirement (EAR) or recommended dietary allowance (RDA) given for most of the essential vitamins and minerals. The current daily AIs for vitamin K for adult women and men are 90 μg and 120 μg respectively. The AI for pregnancy and lactation is 90 μg. For infants up to 12 months the AI is 2–2.5 μg, and for children aged 1 to 18 years the AI increases with age from 30 to 75 μg. As for safety, the FNB also sets tolerable upper intake levels (known as ULs) for vitamins and minerals when evidence is sufficient. In the case of vitamin K no UL is set, as evidence for adverse effects is not sufficient. Collectively EARs, RDAs, AIs and ULs are referred to as dietary reference intakes.
For U.S. food and dietary supplement labeling purposes, the amount in a serving is expressed as a percentage of daily value (%DV). For vitamin K labeling purposes the daily value was 80 μg, but as of May 2016 it has been revised upwards to 120 μg. A table of the pre-change adult daily values is provided at Reference Daily Intake (Table <span id=”MathJax-Element-1-Frame” class=”MathJax” style=”display: inline-table; font-style: normal; font-weight: normal; line-height: normal; font-size: 14.4px; text-indent: 0px; text-align: left; text-transform: none; letter-spacing: normal; word-spacing: normal; overflow-wrap: normal; white-space: nowrap; float: none; direction: ltr; max-width: none; max-height: none; min-width: 0px; min-height: 0px; border: 0px; padding: 0px; margin: 0px; position: relative;” tabindex=”0″ role=”presentation” data-mathml=”7.2D.1″>7.2D.1
7.2D.1). Food and supplement companies have until 28 July 2018 to comply with the change.
Deficiency
Average diets are usually not lacking in vitamin K, and primary deficiency is rare in healthy adults. Newborn infants are at an increased risk of deficiency. Other populations with an increased prevalence of vitamin K deficiency include those who suffer from liver damage or disease (e.g. alcoholics), cystic fibrosis, or inflammatory bowel diseases, or have recently had abdominal surgeries. Secondary vitamin K deficiency can occur in people with bulimia, those on stringent diets, and those taking anticoagulants. Other drugs associated with vitamin K deficiency include salicylates, barbiturates, and cefamandole, although the mechanisms are still unknown. Vitamin K1 deficiency can result in coagulopathy, a bleeding disorder. Symptoms of K1 deficiency include anemia, bruising, nosebleeds and bleeding of the gums in both sexes, and heavy menstrual bleeding in women.
| Food | Serving size | Vitamin K1 (μg) |
Food | Serving size | Vitamin K1 (μg) |
|
|---|---|---|---|---|---|---|
| Kale, cooked | 1⁄2 cup | 531 | Parsley, raw | 1⁄4 cup | 246 | |
| Spinach, cooked | 1⁄2 cup | 444 | Spinach, raw | 1 cup | 145 | |
| Collards, cooked | 1⁄2 cup | 418 | Collards, raw | 1 cup | 184 | |
| Swiss chard, cooked | 1⁄2 cup | 287 | Swiss chard, raw | 1 cup | 299 | |
| Mustard greens, cooked | 1⁄2 cup | 210 | Mustard greens, raw | 1 cup | 279 | |
| Turnip greens, cooked | 1⁄2 cup | 265 | Turnip greens, raw | 1 cup | 138 | |
| Broccoli, cooked | 1 cup | 220 | Broccoli, raw | 1 cup | 89 | |
| Brussels sprouts, cooked | 1 cup | 219 | Endive, raw | 1 cup | 116 | |
| Cabbage, cooked | 1⁄2 cup | 82 | Green leaf lettuce | 1 cup | 71 | |
| Asparagus | 4 spears | 48 | Romaine lettuce, raw | 1 cup | 57 | |
| Table from “Important information to know when you are taking: Warfarin (Coumadin) and Vitamin K”, Clinical Center, National Institutes of Health Drug Nutrient Interaction Task Force. | ||||||
Vitiman A References
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes: Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron Manganese, Molybdenium, Nickel, Silicon, Vanadium, and Zinc. National Academy Press. Washington, DC, 2001. PMID: 25057538 www.ncbi.nlm.nih.gov/pubmed/25057538.
- Mason JB. Vitamins, trace minerals, and other micronutrients. In: Goldman L, Schafer AI, eds. Goldman’s Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier Saunders; 2011:chap 225.
- Salwen MJ. Vitamins and trace elements. In: McPherson RA, Pincus MR, eds. Henry’s Clinical Diagnosis and Management by Laboratory Methods. 22nd ed. Philadelphia, PA: Elsevier Saunders; 2011:chap 26.
A.D.A.M., Inc. is accredited by URAC, also known as the American Accreditation HealthCare Commission (www.urac.org). URAC’s accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.’s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics and subscribes to the principles of the Health on the Net Foundation (www.hon.ch).
Contributers
- Wikipedia
