You probably do not think too much about what actually happens to the food you eat. This section will describe in depth how what you eat is digested. The desired end result for the learner will be an integrated understanding of the process. This will require higher levels of thinking, but will prove to be well worth it in the end.
Sections:
- 3.1 Digestion at a Glance
- 3.2 Mouth to the Stomach
- 3.3 Stomach
- 3.4 Small Intestine
- 3.5 Macronutrient Digestion Review
- 3.6 Large Intestine
Digestion at a Glance

Figure 3.11 A number of organs are involved in digestion, which collectively are referred to as the digestive system1.
Digestion is the process of breaking down food to be absorbed or excreted. There are two types of digestion in the body; mechanical and chemical. Mechanical digestion involves physically breaking food down into smaller pieces, usually through muscle contractions.
Chemical digestion uses enzymes or other chemicals to break of food into smaller nutrients. This generally involves the breaking of chemical bonds in the process.
Required Web Link
The gastrointestinal (GI or digestive) tract, the passageway through which our food travels, is a “tube within a tube.” The trunk of our body is the outer tube and the GI tract is the interior tube, as shown below. Thus, even though the GI tract is within the body, the actual interior of the tract is technically outside of the body. This is because the contents have to be absorbed into the body. If it’s not absorbed, it will be excreted and never enter the body itself. It’s as if you never consumed it.

Figure 3.12 The digestive tract, also known as the gastrointestinal tract, is a “tube within a tube”
The organs that form the gastrointestinal tract (e.g., mouth, esophagus, stomach, small intestine, large intestine (aka colon), rectum, and anus) come into direct contact with the food or digestive contents.

Figure 3.13 The gastrointestinal or digestive tract2
The journey through the gastrointestinal tract starts in the mouth and ends in the anus as shown below:
Mouth –> Esophagus –> Stomach –> Small Intestine –> Large Intestine –> Rectum –> Anus
In addition to the GI tract, there are a number of accessory organs (e.g. salivary glands, pancreas, gallbladder, and liver) that play an integral role in digestion. The accessory organs do not come directly in contact with food or digestive contents, but still play a crucial role in the digestive process.

Figure 3.14 Digestion accessory organs1
In addition to the digestive and accessory organs, there are a number of enzymes that are involved in digestion. We will go through each one in detail later, but this table should help give an overview of which enzymes are active at each location of the GI tract.
|
Location |
Enzyme/Coenzyme |
|
Mouth |
Salivary amylase Lingual lipase |
|
Stomach |
Pepsin |
|
Pancreas
Small Intestine |
Pancreatic amylase Brush border disaccharidases Pancreatic lipase Phospholipase A2 Cholesterol esterase Proteases Brush border peptidases |
References & Links
- http://www.wpclipart.com/medical/anatomy/digestive/Digestive_system_diagram_page.png.html
-
http://commons.wikimedia.org/wiki/File:Digestivetract.gif
Video
Enzymes and Digestion – http://www.youtube.com/watch?v=bNMsNHqxszc
Mouth to the Stomach
Digestion begins in the mouth, both mechanically and chemically. Mechanical digestion in the mouth consists of mastication, or the chewing and grinding of food into smaller pieces. The salivary glands release saliva, mucus, and three enzymes: salivary amylase, lingual lipase, and lysozyme.

Figure 3.21 The mouth
Salivary amylase cleaves the glycosidic bonds in the starch molecules, amylose and amylopectin. Overall however, this enzyme accounts for a minor amount of carbohydrate digestion.
Lysozyme helps break down bacteria cell walls to prevent a possible infection. Another enzyme, lingual lipase, is also released in the mouth. Although it is released in the mouth, it is most active in the stomach where it preferentially cleaves short-chain fatty acids. Lingual lipase has a small role in digestion in adults, but may be important for infants to help break down triglycerides in breast milk2.
Swallowing (a.k.a Deglutition)
Now that the food has been thoroughly chewed and formed into a bolus (a small rounded mass of chewed food), it can proceed down the throat to the next stop in digestion. It will move down the pharynx where it reaches a “fork in the road”, with the larynx as one road and the esophagus as the other. The esophagus road leads to the stomach; this is the direction that food should go (see figure 3.22). The other road, through the larynx, leads to the trachea and ultimately the lungs. This is definitely not where you want your food or drink going, as this is the pathway for the air you breathe.

Figure 3.22 Cross section of face. The epiglottis covers larynx to prevent food and drink from entering the lungs
Fortunately, our body was designed in such a way that a small flap, called the epiglottis, covers the opening to the trachea during swallowing. It directs the food down the correct road as shown below.

Figure 3.23 Epiglottis is like a traffic cop guiding food down the correct digestion road.
Esophagus
Before being correctly guided into the esophagus, the bolus of food will travel through the upper esophageal sphincter. Sphincters are circular muscles that are found throughout the gastrointestinal tract that essentially serve as gates between the different sections. Once in the esophagus, wave-like muscular movements, known as peristalsis, occur, as shown in the animation and video in the links below. Peristalsis occurs throughout the digestive tract with the purpose of moving food along the tract.
Required Web Links Peristalsis Animation Video: Peristalsis (0:57)
At the end of the esophagus, the bolus will encounter the lower esophageal sphincter, also known as the cardiac sphincter due to its proximity to the heart. This sphincter keeps the harmful acids of the stomach out of the esophagus. However, in many people this sphincter is leaky, which allows stomach acid to reflux, or creep up, the esophagus. Stomach acid is very acidic (has a low pH). The ruler below will give you an idea of just how acidic the stomach is. Notice that the pH of gastric (term used to describe the stomach) fluid is lower (more acidic) than any of the listed items besides battery acid.

Figure 3.24 pH of some common items4
The leaking of the very acidic gastric contents results in a burning sensation commonly referred to as “heartburn.” If this occurs more than twice per week and is severe, the person may have gastroesophageal reflux disease (GERD). The following videos explain more about these conditions.
Required Web Links
Video: Acid Reflux (1:28) Video: GERD 101 (0.55)
|
Macronutrient |
Action |
|---|---|
|
Carbohydrates |
Salivary amylase cleaves glycosidic bonds |
|
Lipids |
Lingual lipase begins digestion of triglycerides |
|
Protein |
None |
References & Links
- Alan Hoofring, http://visualsonline.cancer.gov/details.cfm?imageid=4371
- Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ, editors. (2006) Modern Nutrition in Health and Disease. Baltimore, MD: Lippincott Williams & Wilkins.
-
http://en.wikipedia.org/wiki/File:Illu01_head_neck.jpg
- http://upload.wikimedia.org/wikipedia/commons/4/46/PH_scale.png
Link
Peristalsis – http://en.wikipedia.org/wiki/File:Peristalsis.gif
Videos
Peristalsis Animation – http://www.youtube.com/watch?v=o18UycWRsaA Acid Reflux – https://www.youtube.com/watch?v=SW-QfyDSY5I
GERD 101 – http://www.youtube.com/watch?v=FqdOvZkrSYk&feature=rec-lis-watch-cur_emp- farside_rn
Stomach
After going through the lower esophageal sphincter, food enters the stomach. Our stomach is involved in both chemical and mechanical digestion. Mechanical digestion occurs as the stomach churns and grinds food into a semisolid substance called chyme (partially digested food).
There are four main regions in the stomach: the cardia, fundus, body, and pylorus (see Figure 3.31 below). The cardia (or cardiac region) is the point where the esophagus connects to the stomach and through which food passes into the stomach. Located inferior to the diaphragm, above and to the left of the cardia, is the dome-shaped fundus. Below the fundus is the body, the main part of the stomach. The funnel-shaped pylorus connects the stomach to the duodenum. The wider end of the funnel, the pyloric antrum, connects to the body of the stomach. The narrower end is called the pyloric canal, which connects to the duodenum. The smooth muscle pyloric sphincter is located at this latter point of connection and controls stomach emptying. In the absence of food, the stomach deflates inward, and its mucosa and submucosa fall into a large fold called a rugae6. These rugae increase the surface area inside the stomach, which aids the digestive process.

Figure 3.31 The stomach has four major regions: the cardia, fundus, body, and pylorus. The addition of an inner oblique smooth muscle layer gives the muscularis the ability to vigorously churn and mix food.
The lining of the stomach is made up of four different layers of tissue. For the purposes of this discussion, we will focus on only the innermost layer. The mucosa is the innermost layer of the stomach (closest to stomach cavity) as shown in the figure below.

Figure 3.32 The anatomy of the stomach1
The mucosa is not a flat surface. Instead, its surface is lined by gastric pits, as shown in the figure 3.33 below.

Figure 3.33 Gastric pits2
Gastric pits are indentations in the stomach’s surface that are lined by four different types of cells (see figure 3.34 for names and locations).

Figure 3.34 Blowup of mucosa to show the structure of gastric pits1
The following video is a nice introduction to gastric pits and talks about chief and parietal cells that are covered in more detail below.
Required Web Link
At the bottom of the gastric pit are the gastric enteroendocrine cells (G cells) that secrete the hormone gastrin. Gastrin stimulates the parietal and chief cells that are found above the G cells. The chief cells secrete the pepsinogen. Pepsinogen is the inactive precursor that must be altered to form the active enzyme, pepsin. The parietal cells secrete hydrochloric acid (HCl), which lowers the pH of the gastric juice (water + enzymes + acid). The HCl also inactivates salivary amylase and catalyzes the conversion of the inactive pepsinogen to its active form, known as pepsin. Finally, at the top of the pits are the neck cells (specialized goblet cells) that secrete mucus to prevent the gastric juice from digesting or damaging the stomach mucosa3. The table below summarizes the actions of the different cells in the gastric pits.
|
Type of Cell |
Secrete |
|
Neck (Goblet) |
Mucus |
|
Chief |
Pepsinogen |
|
Parietal |
HCl |
|
G |
Gastrin |
The figure below shows the action of all these different secretions in the stomach.

Figure 3.35 The action of gastric secretions in the stomach
To reiterate, the figure above illustrates that the neck cells of the gastric pits secrete mucus to protect the mucosa of the stomach from essentially digesting itself. Gastrin from the G cells stimulates the parietal and chief cells to secrete HCl and enzymes, respectively.
The HCl in the stomach denatures salivary amylase and other proteins by breaking down the structure and, thus, the function of it. HCl also converts pepsinogen to the active enzyme pepsin. Pepsin is a protease, meaning that it cleaves the peptide bonds in proteins. It breaks down the proteins in food into individual peptides (shorter segments of amino acids).
The chyme will then leave the stomach in small amounts and enter the small intestine via the pyloric sphincter (shown below). Full emptying of the stomach takes about 2-4 hours.

Figure 3.36 Cross section of the stomach showing the pyloric sphincter5
|
Chemical or Enzyme |
Action |
|
Gastrin |
Stimulates chief cells to release pepsinogen Stimulates parietal cells to release HCl |
|
HCl |
Denatures salivary amylase Denatures proteins Facilitates the conversion of pepsinogen to pepsin |
|
Pepsin |
Cleaves proteins to peptides |
References & Links
-
https://en.wikipedia.org/wiki/Stomach#/media/File:Illu_stomach2.jpg
-
http://en.wikipedia.org/wiki/File:Gray1055.png
- Gropper SS, Smith JL, Groff JL. (2008) Advanced Nutrition and Human Metabolism. Belmont, CA: Wadsworth Publishing.
- Stipanuk MH. (2006) Biochemical, Physiological, & Molecular Aspects of Human Nutrition. St. Louis, MO: Saunders Elsevier.
-
https://en.wikipedia.org/wiki/Pylorus#/media/File:Gray1050.png
- OpenStax, Anatomy & Physiology. OpenStax CNX. Aug 1, 2017 http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.108
Video
Gastric Pits – http://www.youtube.com/watch?v=6hquzCXYlNg
Small Intestine
The small intestine is the primary site of digestion. It is divided into three sections: the duodenum, jejunum, and ileum (shown below). After leaving the stomach, the first part of the small intestine that chyme will encounter is the duodenum.

Figure 3.41 Three sections of the small intestine1
The small intestine consists of many layers, which can be seen in the cross section in Figure 3.42 below.

Figure 3.42 Cross section of the small intestine2
Examining these layers more closely, we are going to focus on the lining of the small intestine, known as the epithelium (see Figure 3.42 above), which comes into contact with the chyme and is responsible for absorption. The lumen is the name of the cavity that is considered “outside the body” that chyme moves through.
The organization of the small intestine is in such a way that it contains circular folds and finger- like projections known as villi. The folds and villi are shown in the next few figures.

Figure 3.43 Folds in the small intestine2
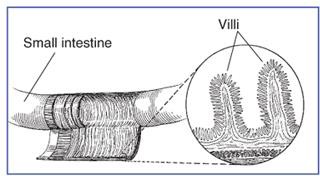
Figure 3.44 Villi in the small intestine3

Figure 3.45 Villi line the surface of the small intestine2,4
If we were to zoom in even closer, we would be able to see that enterocytes (small intestine absorptive cells; a.k.a brush border cells) line villi as shown below. This layer is referred to as the mucosa, and is composed primarily of simple columnar epithelium.
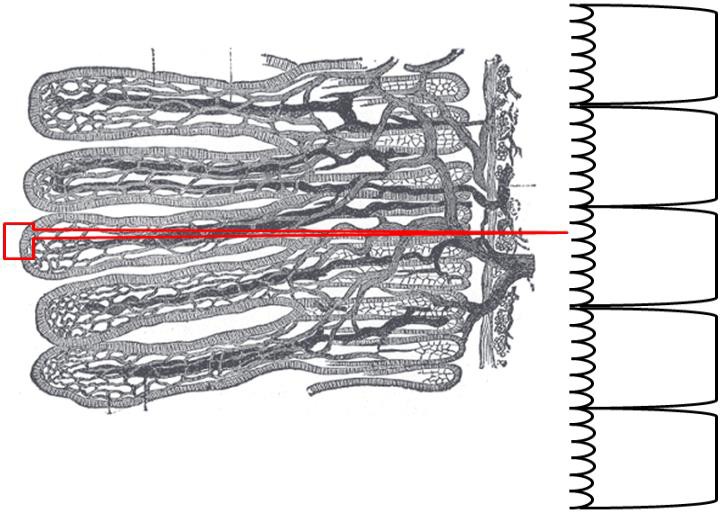
Figure 3.46 Enterocytes line villi4
The side, or membrane, of the enterocyte that faces the lumen is not smooth either. It is lined with microvilli, and is known as the brush border membrane, as shown below.

Figure 3.47 Enterocyte, or small intestinal absorptive cell is lined with microvilli. This lined surface is referred to as the brush border membrane.
Together these features (folds + villi + microvilli) increase the surface area ~600 times versus if it was a smooth tube5. (Note: the symbol ~ is used in place of the word “approximately.” You will see it used other places in this text as well.) More surface area leads to more contact between the chyme and the enterocytes, and thus, increased absorption.
Finally, the surface of the cells on the microvilli are covered with proteins, which helps to catch a molecule-thin layer of water within itself. This layer, called the “unstirred water layer,” has a number of functions in absorption of nutrients, and will have a direct impact on fat absorption as we will see later6.

Figure 3.48 Unstirred water layer
Now that you have learned about the anatomy of the small intestine, the following subsections go through the different digestive processes that occur there.
Subsections:
- 3.41 Digestive Hormones, Accessory Organs, & Secretions
- 3.42 Carbohydrate Digestion in the Small Intestine
- 3.43 Protein Digestion in the Small Intestine
- 3.44 Lipid Digestion in the Small Intestine
References & Links
-
http://commons.wikimedia.org/wiki/Image:Illu_small_intestine_catal%C3%A0.png
- Author unknown, NCI, http://visualsonline.cancer.gov/details.cfm?imageid=1781
- http://digestive.niddk.nih.gov/ddiseases/pubs/celiac/
-
http://commons.wikimedia.org/wiki/Image:Gray1061.png
- Byrd-Bredbenner C, Moe G, Beshgetoor D, Berning J. (2009) Wardlaw’s Perspectives in Nutrition. New York, NY: McGraw-Hill.
- http://www.newworldencyclopedia.org/entry/Small_intestine
Digestive Hormones, Accessory Organs & Secretions
Before we go into the digestive details of the small intestine, it is important that you have a basic understanding of the anatomy and physiology of the following digestion accessory organs: pancreas, liver, and gallbladder. Digestion accessory organs assist in digestion, but are not part of the gastrointestinal tract. How are these organs involved?
Upon entering the duodenum, the chyme causes the release of two hormones from the small intestine: secretin and cholecystokinin (CCK) in response to acid and fat, respectively. These
hormones have multiple effects on different tissues. In the pancreas, secretin stimulates the secretion of bicarbonate (HCO3), while CCK stimulates the secretion of digestive enzymes. The bicarbonate and digestive enzymes released together are collectively known as pancreatic juice, which travels to the small intestine, as shown below.

Figure 3.411 The hormones secretin and CCK stimulate the pancreas to secrete pancreatic juice1
In addition, CCK also stimulates the contraction of the gallbladder causing the secretion of stored bile into the duodenum.
Pancreas
The pancreas is found behind the stomach and just above the transverse colon (part of the large intestine discussed later in this chapter). It is a tadpole-shaped organ consisting of a head, body, and tail. It is a unique organ containing both endocrine and exocrine portions. The smaller, endocrine (hormone-producing) portions contain alpha, beta, delta, and PP cells that secrete the hormones glucagon, insulin, somatostatin, and pancreatic polypeptide respectively. These cells are clustered in groups known as pancreatic islets (traditionally referred to as the Islets of Langerhans). However, the vast majority of the pancreas is made up of grape-like clusters of exocrine cells known as acini (singular = acinus). The cells composing each acinus are known as acinar cells. These acinar cells are responsible for producing enzyme-rich pancreatic juice. Pancreatic juice is released into small ducts that continually merge to form a large main pancreatic duct which delivers pancreatic juice from the pancreas to the duodenum, merging with the common bile duct (from the liver & gallbladder) along the way. The release of pancreatic juice, and bile, is controlled by the hepatopancreatic sphincter. The following video does a nice job of showing and explaining the function of the different pancreatic cells.

Figure 3.412 The pancreas has a head, a body, and a tail. It delivers pancreatic juice to the duodenum through the pancreatic duct5.
Required Web Link
Video: The Pancreas (First 53 seconds)
In addition to pancreatic hormones and enzymes, the pancreas releases bicarbonate. Bicarbonate is a base (high pH) meaning that it can help neutralize an acid (such as gastric juice.) You can find sodium bicarbonate (NaHCO3, baking soda) on the ruler below to get an idea of its pH.

Figure 3.413 pH of some common items2
The main digestive enzymes in pancreatic juice are listed in the table below. Their function will be discussed further in later subsections.
|
Enzyme |
|
Pancreatic amylase |
|
Proteases |
|
Pancreatic Lipase |
|
Phospholipase A2 |
|
Cholesterol Esterase |
Liver
The liver is the largest internal, and the most metabolically active, organ in the body. The figure below shows the liver and the other accessory organs position relative to the stomach.

Figure 3.414 Location of digestion accessory organs relative to the stomach3
The liver is made up two major types of cells. The primary liver cells are hepatocytes, which carry out most of the liver’s functions. Hepatic is another term for liver. For example, if you are going to refer to liver concentrations of a certain nutrient, these are often reported as hepatic concentrations. The other major cell type is the hepatic stellate (also known as Ito) cells. These are fat storing cells in the liver.
The liver’s major role in digestion is to produce bile. This is a greenish-yellow fluid that is composed primarily of bile acids, but also contains cholesterol, phospholipids, and the pigments bilirubin and biliverdin. Bile acids are synthesized from cholesterol. The two primary bile acids are chenodeoxycholic acid and cholic acid. In the same way that fatty acids are found in the form of salts, these bile acids can also be found as salts. Because of this, these bile salts are often seen in texts with an (-ate) ending (chenodeoxycholate and cholate) indicating they are in the salt form.
Bile acids, much like phospholipids, have both hydrophobic and hydrophilic portions. This makes them excellent emulsifiers that are instrumental in fat digestion. Bile is then transported to the gallbladder.
Gallbladder
The gallbladder is a small, sac-like organ found just off the liver (see figure 3.413 above). Its primary function is to store and concentrate bile made by the liver. The bile is then transported to the duodenum through the common bile duct.
Why do we need bile?
Bile is important because fat is hydrophobic, but the environment in the lumen of the small intestine is watery. In addition, there is an unstirred water layer that fat must cross to reach the enterocytes in order to be absorbed.

Figure 3.415 Fat is not happy alone in the watery environment of the small intestine.
Triglycerides naturally form large triglyceride droplets to keep the interaction with the watery environment to a minimum. Picture the large droplets of cooking oil that form when you add it to water. This is inefficient for digestion, because enzymes cannot access the interior of the droplet. Bile acts as an emulsifier, or detergent. It, along with phospholipids, breaks the large triglyceride droplets into smaller triglyceride droplets that increase the surface area accessible for triglyceride digestive enzymes, as shown below.

Figure 3.416 Bile acids and phospholipids facilitate the production of smaller triglyceride droplets.
Secretin and CCK also control the production and secretion of bile. Secretin stimulates the flow of bile from the liver to the gallbladder. CCK stimulates the gallbladder to contract, causing bile to be secreted into the duodenum, as shown in Figure 3.417.

Figure 3.417 Secretion stimulates bile flow from liver; CCK stimulates the gallbladder to contract3
References & Links
- Don Bliss, NCI, http://visualsonline.cancer.gov
-
http://upload.wikimedia.org/wikipedia/commons/4/46/PH_scale.png 3.http://www.wpclipart.com/medical/anatomy/digestive/Digestive_system_diagram_page.png.html
-
OpenStax, Anatomy & Physiology. OpenStax CNX. Aug 1, 2017 http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.108
Video
The Pancreas – http://www.youtube.com/watch?v=j5WF8wUFNkI
Carbohydrate Digestion in the Small Intestine
The small intestine is the primary site of carbohydrate digestion. Pancreatic amylase is the primary carbohydrate digesting enzyme. Pancreatic amylase, like salivary amylase, cleaves the glycosidic bonds of carbohydrates, reducing them to simpler carbohydrates, such as glucose, maltose, maltotriose, and α-dextrin (an oligosaccharide containing 1 or more glycosidic bonds which pancreatic amylase unable to cleave1).
The pancreatic amylase products, along with the disaccharides sucrose and lactose, then move to the surface of the enterocyte.
Here, the brush border enzyme α-dextrinase starts working on α-dextrin, breaking off one glucose unit at a time. Three other brush border enzymes hydrolyze sucrose, lactose, and maltose into monosaccharides. Sucrase splits sucrose into one molecule of fructose and one molecule of glucose; maltase breaks down maltose into two glucose molecules; and lactase breaks down lactose into one molecule of glucose and one molecule of galactose2. Insufficient lactase can lead to lactose intolerance (discussed in a later chapter.) The products from these brush border enzymes are the single monosaccharides glucose, fructose, and galactose that are ready for absorption into the enterocyte1.

Figure 3.423 Disaccharidases on the outside of the enterocyte.

Figure 3.424 Carbohydrates are broken down into their monomers in a series of steps2.
References & Links
- Gropper SS, Smith JL, Groff JL. (2008) Advanced Nutrition and Human Metabolism. Belmont, CA: Wadsworth Publishing.
- OpenStax, Anatomy & Physiology. OpenStax CNX. Aug 1, 2017 http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.108
Protein Digestion in the Small Intestine
The small intestine is the major site of protein digestion by proteases (enzymes that cleave proteins). The pancreas secretes a number of proteases into the duodenum where they must be activated before they can cleave peptide bonds1. This activation occurs through an activation cascade. A cascade is a series of reactions in which one step activates the next in a sequence that results in an amplification of the response. An example of a cascade is shown below.

Figure 3.431 An example of a cascade, with one event leading to many more events
In the above example, A activates B, B activates C, D, and E, C activates F and G, D activates H and I, and E activates K and L. Cascades also help to serve as control points for certain process. In the protease cascade, the activation of B is really important because it starts the cascade.
The protease activation scheme starts with the enzyme enteropeptidase (secreted from the intestinal brush border) that converts trypsinogen (released by the pancreas) to trypsin. Trypsin can activate all the proteases (including itself) as shown in the 2 figures below.

Figure 3.432 Protease activation cascade

Figure 3.433 The protease activation cascade
The products of the action of the activated proteases on proteins are dipeptides, tripeptides, and individual amino acids, as shown below.

Figure 3.434 Products of pancreatic proteases
At the brush border, much like disaccharidases, there are peptidases that cleave some peptides down to amino acids. Not all peptides are cleaved to individual amino acid, because small
peptides can be taken up into the enterocyte, thus, the peptides do not need to be completely broken down to individual amino acids. Thus, the end products of protein digestion are primarily dipeptides and tripeptides, along with individual amino acids.

Figure 3.435 Peptidases are produced by the brush border to cleave some peptides into amino acids
References & Links
1. Gropper SS, Smith JL, Groff JL. (2008) Advanced Nutrition and Human Metabolism. Belmont, CA: Wadsworth Publishing.
Lipid Digestion in the Small Intestine
The small intestine is the major site for lipid digestion. There are specific enzymes for the digestion of triglycerides, phospholipids, and the removal of esters from cholesterol. We will look at each in this section. Refer back to sections 2.35, 2.36, and 2.36 for a review of these structures.
Triglycerides
The pancreas secretes pancreatic lipase into the duodenum as part of pancreatic juice. This major triglyceride digestion enzyme preferentially cleaves two fatty acids from triglycerides. This cleavage results in the formation of a monoglyceride and two free fatty acids as shown in Figures 3.441 & 3.442.

Figure 3.441 Pancreatic lipase cleaves the sn-1 and sn-3 fatty acids of triglycerides
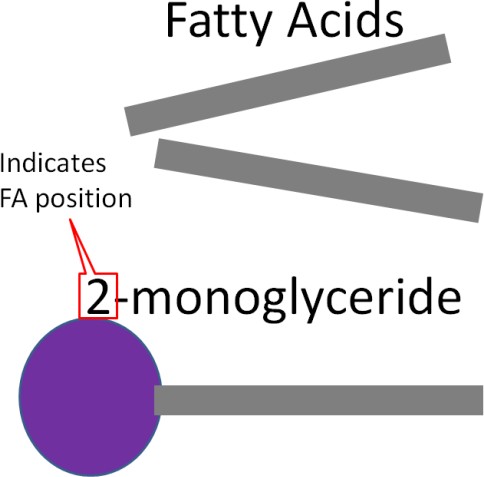
Figure 3.442 The products of pancreatic lipase are a 2-monoglyceride and two free fatty acids
Phospholipids
The enzyme phospholipase A2 cleaves the fatty acid of lecithin, producing lysolecithin and a free fatty acid. This is depicted in Figures 3.444 & 3.445.

Figure 3.444 Phospholipase A2 cleaves the C-2 fatty acid of lecithin

Figure 3.445 Products of phospholipase A2 cleavage
Cholesterol Esters
The fatty acid in cholesterol esters is cleaved by the enzyme, cholesterol esterase, producing cholesterol and a free fatty acid.

Figure 3.446 Cholesterol esterase cleaves fatty acids off of cholesterol

Figure 3.447 Products of cholesterol esterase
Formation of Mixed Micelles
If nothing else happened at this point, the monoglycerides and fatty acids produced by pancreatic lipase would form micelles. The hydrophilic heads would be outward and the fatty acids would be buried on the interior. These micelles are not sufficiently water-soluble to cross the unstirred water layer to get to the brush border of enterocytes. Thus, mixed micelles are formed containing cholesterol, bile acids, and lysolecithin in addition to the monoglycerides and fatty acids, as illustrated below1.

Figure 3.448 Normal (left) and mixed (right) micelles
Mixed micelles are more water-soluble, allowing them to cross the unstirred water layer to the brush border of enterocytes for absorption.

Figure 3.449 Mixed micelles can cross the unstirred water layer for absorption into the enterocytes
After digestion of carbohydrates, proteins, and fats is complete, the products below are ready for uptake into the enterocyte. This will be discussed in the next chapter.

Figure 3.55 Macronutrient digestion products ready for uptake into the enterocyte
References & Links
1. Gropper SS, Smith JL, Groff JL. (2008) Advanced nutrition and human metabolism. Belmont, CA: Wadsworth Publishing.
3.6 The Large Intestine
We have now reached a fork in the digestive road. We could follow the uptake of the digested compounds into the enterocyte or we could finish following what has escaped digestion and is going to continue into the large intestine. Obviously from the title of this section we are going to do the latter. As we learned previously, fiber is a crude term for what has survived digestion and has reached the large intestine.

Figure 3.61 The fork in the road between finishing digestion in the colon and absorption into the enterocyte
The ileocecal valve is the sphincter between the ileum (hence ileo– in ileocecal valve), and the large intestine. This name should make more sense as we go through the anatomy of the large intestine.

Figure 3.62 The ileocecal valve1
The large intestine consists of the colon, the rectum, and the anus. The colon can be further divided into the cecum (hence the –cecal in ileocecal valve), ascending colon, transverse colon, descending colon, and sigmoid colon as shown below.

Figure 3.63 Anatomy of the large intestine and rectum2
The large intestine is responsible for absorbing the remaining water and electrolytes (sodium, potassium, and chloride) in chyme. By removing water, the unabsorbed chyme is converted into a more solid form (feces) which is then excreted via defecation. The large intestine contains large amounts of microorganisms like those shown in the figure below.

Figure 3.64 Magnified image of bacteria3
The large intestine can also be referred to as the gut. There are a large number of microorganisms found throughout the gastrointestinal tract that collectively are referred to by a variety of names: flora, microflora, biota, or microbiota. Technically, microbiota is the preferred term because flora means “pertaining to plants”. There are 10 times more microorganisms in the gastrointestinal tract than cells in the whole human body4. As can be seen in the figure below, the density of microorganisms increases as you move down the digestive tract.

Figure 3.65 Relative amounts of bacteria in selected locations of the GI tract. cfu/ml = colony forming unit, a measure of the number of live microorganisms in 1 mL of digestive sample5,6
As described in the fiber sections, there are two different fates for fiber once it reaches the large intestine. The fermentable, viscous fiber is fermented by bacteria. Fermentation is the metabolism of compounds by the microorganisms in the gut. An example of fermentation is the utilization of the oligosaccharides raffinose and stachyose by microorganisms that results in the production of gas, which can lead to flatulence. Additionally, some bile acids are fermented by microorganisms to form secondary bile acids that can be reabsorbed. These secondary bile acids represent approximately 20% of the total bile acids in our body. Fermentable fibers can also be used to form short-chain fatty acids that can then be absorbed and used by the body.
Conversely, the non-fermentable, non-viscous fiber is not really altered and will be a component of feces, that is then excreted through the rectum and anus via defecation. This process involves both an internal and external sphincter that are shown in figure 3.63 above.
References & Links
-
https://commons.wikimedia.org/wiki/File:Gray1075.png
-
http://en.wikipedia.org/wiki/Image:Illu_intestine.jpg
-
http://commons.wikimedia.org/wiki/Image:Cholera_bacteria_SEM.jpg
- Guarner F, Malagelada J. (2003) Gut flora in health and disease. The Lancet 361(9356): 512.
- DiBaise J, Zhang H, Crowell M, Krajmalnik-Brown R, Decker, et al. (2008) Gut microbiota and its possible relationship with obesity. Mayo Clin Proc 83(4): 460.
- Adapted from: http://www.wpclipart.com/medical/anatomy/digestive/Digestive_system_diagram_page.png.h tml
3.61 Probiotics & Prebiotics
Recently there has been increased attention given to the potential of a person’s microbiota to impact health. This is because there are beneficial and non-beneficial bacteria inhabiting our gastrointestinal tracts. Thus, theoretically, if you can increase the beneficial, or decrease the non-beneficial bacteria, there may be improved health outcomes. In response to this, probiotics and prebiotics have been identified/developed. A probiotic is a live microorganism that is consumed, and colonizes in the body as shown in Figure 3.611.

Figure 3.611 Probiotics the consumption of the bacteria itself
A prebiotic is a non-digestible food component that selectively stimulates the growth of beneficial intestinal bacteria. An example of a prebiotic is inulin (this is not the same as, or related to, the hormone insulin that you may be familiar with), which is shown in the figure below.

Figure 3.612 Inulin, an indigestible food component that is a commonly used prebiotic The net result is the same for both prebiotics and probiotics, an improvement in the beneficial/non-beneficial bacteria ratio.

Figure 3.613 An effective prebiotic or probiotic should result in an increase in the beneficial bacteria
The following video does a nice job of explaining and illustrating how probiotics work. The NCCAM website is a good source of information if you have further questions on the topic.
Required Web Links
Video: Probiotics (3:40) NCCAM: Probiotics
Some common examples of probiotic foods are sauerkraut, kimchi, kefir, and yogurts containing live cultures such as DanActive® and Activia®.
Required Web Links
DanActive® Activia®
It should be notes that the claims companies have made about their probiotic products have come under scrutiny. Dannon settled with the US Federal Trade Commission to drop claims that its probiotic products will help prevent colds or alleviate digestive problems, as seen in the top link below. General Mills also settled a lawsuit that accused them of a falsely advertising the digestive benefits of Yo-Plus, a product it no longer sells, as seen in the second link.
Required Web Link
New Campaign Markets Activia to Wider Audience General Mills Settles Yo-Plus Lawsuit
Some examples of prebiotics include the previously mentioned inulin, fructose-containing oligosaccharides and polysaccharides, and resistant starch. These are found in a number of foods including onions, leaks, sprouted whole grains, seeds, and berries.3
Resistant starch is so named because it is a starch that is resistant to digestion. As a result, it arrives in the colon to be fermented.
References & Links
-
http://en.wikipedia.org/wiki/File:Inulin_strukturformel.png
- Douglas L, Sanders M. (2008) Probiotics and prebiotics in dietetics practice. American Dietetic Association. Journal of the American Dietetic Association 108(3): 510.
- Gut Health 101: Top Prebiotic and Probiotic Foods https://www.betternutrition.com/checkout/prebiotic-probiotic-foods-lists
Links
Activia® – http://www.activia.us.com/
Danimals® – http://www.danimals.com/New Campaign Markets Activia to Wider Audience – http://www.nytimes.com/2014/01/06/business/media/new-campaign-markets-activia-to- wider-audience.html?_r=0
General Mills Settles Yo-Plus Lawsuit – http://www.foodbusinessnews.net/articles/news_home/Site_News/2013/02/General_Mills_se ttles_Yo-Plus.aspx?ID={40F62478-1AA4-49DF-9330-E41E19E946D0}&cck=1
Video
Probiotics – http://www.youtube.com/watch?v=2k8Puxz54FQ&NR=1
