One of the major functions of vitamin D is to assist in maintaining blood calcium concentrations. The other major regulators of blood calcium levels are 2 hormones: parathyroid hormone (PTH) and calcitonin, which are released from the parathyroid glands and thyroid glands, respectively. Bone serves as the calcium depot, or reservoir, if there is a sufficient concentration in the body. In bone, calcium is found in hydroxyapatite crystals on a collagen matrix.
The chemical formula of hydroxyapatite is:
Ca10(PO4)6(OH)2
Calcium and phosphorus are either jointly deposited (deposition) or jointly liberated (resorption) from bone hydroxyapatite to maintain/achieve blood calcium concentrations. Osteoblasts are bone cells that are responsible for bone formation or depositing hydroxyapatite. Osteoclasts are the bone cells that are responsible for breaking down or resorption of bone. An easy way to remember the function of these cells is:
Osteoblasts “build” bone
Osteoclasts “chew” bone
Bone resorption is the process of liberating calcium and phosphorus from hydroxyapatite.
Bone deposition is the process of depositing calcium and phosphorus in bone as hydroxyapatite.
Response to Low Blood Calcium
The parathyroid senses low blood calcium concentrations and releases PTH. These steps are designed to maintain consistent blood calcium levels, but also affects phosphate (phosphorus) levels. PTH has 3 effects:
1. Increases bone resorption
2. Decreases calcium and increases phosphorus urinary excretion
3. Increases 1,25(OH)2D activation in the kidney1,2
The first effect of PTH is increased bone resorption. Hydroxyapatite must be broken down to release both calcium and phosphate. This effect is illustrated below.

Figure 12.131 PTH effect 1: increased bone resorption3
The second effect of PTH is decreased calcium excretion in urine. This is a result of increased calcium reabsorption by the kidney before it is excreted in urine. Kidney phosphate reabsorption is decreased, meaning the net effect is less calcium, but more phosphate in urinary excretion, as shown in the figure below.

Figure 12.132 PTH effect 2: decreased calcium, increased phosphorus excretion3
The 3rd effect of PTH is that it increases 1,25(OH)2D activation in the kidney, by increasing 1alpha-hydroxylase levels. The 1,25(OH)2D then increases calcium and phosphorus absorption in the small intestine to help raise blood calcium levels, as shown below. This mechanism will be discussed in more detail in the vitamin D receptor subsection.
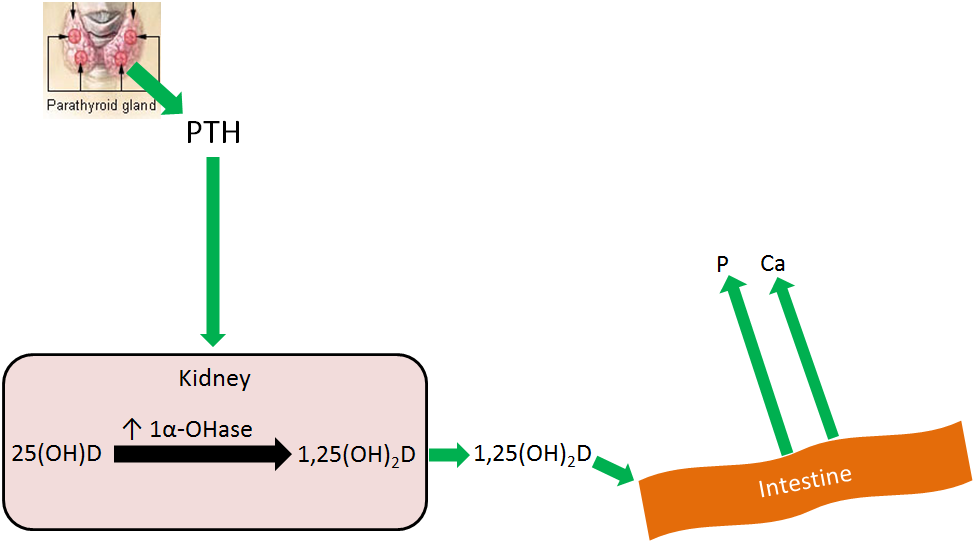
Figure 12.133 PTH effect 3: increased 1,25(OH)2D activation3
Overall PTH causes more calcium and phosphate to be leached from bone, and absorbed from the intestine, into the blood. Coupled with decreased calcium and increased phosphate urinary excretion, means that blood calcium levels rise without a marked rise in phosphate levels, as depicted in the figure below.

Figure 12.134 1,25(OH)2D increased calcium and phosphorus absorption3
References & Links
1. Gropper SS, Smith JL, Groff JL. (2008) Advanced nutrition and human metabolism. Belmont, CA: Wadsworth Publishing.
2. Whitney E, Rolfes SR. (2011) Understanding nutrition. Belmont, CA: Wadsworth Cengage Learning.
3. http://en.wikipedia.org/wiki/File:Illu_thyroid_parathyroid.jpg
Candela Citations
- Kansas State University Human Nutrition Flexbook. Authored by: Brian Lindshield. Provided by: Kansas State University. Located at: http://goo.gl/vOAnR. License: CC BY: Attribution
