Explain the role of muscles in locomotion
Muscle contraction occurs when sarcomeres shorten, as thick and thin filaments slide past each other, which is called the sliding filament model of muscle contraction. ATP provides the energy for cross-bridge formation and filament sliding. Regulatory proteins, such as troponin and tropomyosin, control cross-bridge formation. Excitation–contraction coupling transduces the electrical signal of the neuron, via acetylcholine, to an electrical signal on the muscle membrane, which initiates force production. The number of muscle fibers contracting determines how much force the whole muscle produces.
Learning Objectives
- Classify the different types of muscle tissue and fibers
- Describe the processes of muscle contraction
- Discuss why ATP is necessary for muscle movement
- Identify the role of the brain in muscle movement
- Discuss muscle tension and contraction
Types of Muscle Tissue and Fibers
Muscle cells are specialized for contraction. Muscles allow for motions such as walking, and they also facilitate bodily processes such as respiration and digestion. The body contains three types of muscle tissue: skeletal muscle, cardiac muscle, and smooth muscle (Figure 1).

Figure 1. The body contains three types of muscle tissue: skeletal muscle, smooth muscle, and cardiac muscle, visualized here using light microscopy. Smooth muscle cells are short, tapered at each end, and have only one plump nucleus in each. Cardiac muscle cells are branched and striated, but short. The cytoplasm may branch, and they have one nucleus in the center of the cell. (credit: modification of work by NCI, NIH; scale-bar data from Matt Russell)
Skeletal muscle tissue forms skeletal muscles, which attach to bones or skin and control locomotion and any movement that can be consciously controlled. Because it can be controlled by thought, skeletal muscle is also called voluntary muscle. Skeletal muscles are long and cylindrical in appearance; when viewed under a microscope, skeletal muscle tissue has a striped or striated appearance. The striations are caused by the regular arrangement of contractile proteins (actin and myosin). Actin is a globular contractile protein that interacts with myosin for muscle contraction. Skeletal muscle also has multiple nuclei present in a single cell.
Smooth muscle tissue occurs in the walls of hollow organs such as the intestines, stomach, and urinary bladder, and around passages such as the respiratory tract and blood vessels. Smooth muscle has no striations, is not under voluntary control, has only one nucleus per cell, is tapered at both ends, and is called involuntary muscle.
Cardiac muscle tissue is only found in the heart, and cardiac contractions pump blood throughout the body and maintain blood pressure. Like skeletal muscle, cardiac muscle is striated, but unlike skeletal muscle, cardiac muscle cannot be consciously controlled and is called involuntary muscle. It has one nucleus per cell, is branched, and is distinguished by the presence of intercalated disks.
Skeletal Muscle Fiber Structure
Each skeletal muscle fiber is a skeletal muscle cell. These cells are incredibly large, with diameters of up to 100 µm and lengths of up to 30 cm. The plasma membrane of a skeletal muscle fiber is called the sarcolemma. The sarcolemma is the site of action potential conduction, which triggers muscle contraction. Within each muscle fiber are myofibrils—long cylindrical structures that lie parallel to the muscle fiber. Myofibrils run the entire length of the muscle fiber, and because they are only approximately 1.2 µm in diameter, hundreds to thousands can be found inside one muscle fiber. They attach to the sarcolemma at their ends, so that as myofibrils shorten, the entire muscle cell contracts (Figure 2).

Figure 2. A skeletal muscle cell is surrounded by a plasma membrane called the sarcolemma with a cytoplasm called the sarcoplasm. A muscle fiber is composed of many fibrils, packaged into orderly units.
The striated appearance of skeletal muscle tissue is a result of repeating bands of the proteins actin and myosin that are present along the length of myofibrils. Dark A bands and light I bands repeat along myofibrils, and the alignment of myofibrils in the cell causes the entire cell to appear striated or banded.

Figure 3. A sarcomere is the region from one Z line to the next Z line. Many sarcomeres are present in a myofibril, resulting in the striation pattern characteristic of skeletal muscle.
Each I band has a dense line running vertically through the middle called a Z disc or Z line. The Z discs mark the border of units called sarcomeres, which are the functional units of skeletal muscle. One sarcomere is the space between two consecutive Z discs and contains one entire A band and two halves of an I band, one on either side of the A band. A myofibril is composed of many sarcomeres running along its length, and as the sarcomeres individually contract, the myofibrils and muscle cells shorten (Figure 3).
Myofibrils are composed of smaller structures called myofilaments. There are two main types of filaments: thick filaments and thin filaments; each has different compositions and locations. Thick filaments occur only in the A band of a myofibril. Thin filaments attach to a protein in the Z disc called alpha-actinin and occur across the entire length of the I band and partway into the A band. The region at which thick and thin filaments overlap has a dense appearance, as there is little space between the filaments. Thin filaments do not extend all the way into the A bands, leaving a central region of the A band that only contains thick filaments. This central region of the A band looks slightly lighter than the rest of the A band and is called the H zone (Figure 4). The middle of the H zone has a vertical line called the M line, at which accessory proteins hold together thick filaments. Both the Z disc and the M line hold myofilaments in place to maintain the structural arrangement and layering of the myofibril. Myofibrils are connected to each other by intermediate, or desmin, filaments that attach to the Z disc. The primary component of thin filaments is the actin protein. Two other components of the thin filament are tropomyosin and troponin. Actin has binding sites for myosin attachment. Strands of tropomyosin block the binding sites and prevent actin–myosin interactions when the muscles are at rest. Troponin consists of three globular subunits. One subunit binds to tropomyosin, one subunit binds to actin, and one subunit binds Ca2+ ions.

Figure 4. The sarcomere
Watch this video showing the organization of muscle fibers.
Sliding Filament Model of Contraction
When a muscle contracts, the actin is pulled along myosin toward the center of the sarcomere until the actin and myosin filaments are completely overlapped. In other words, for a muscle cell to contract, the sarcomere must shorten. However, thick and thin filaments—the components of sarcomeres—do not shorten. Instead, they slide by one another, causing the sarcomere to shorten while the filaments remain the same length. The sliding filament theory of muscle contraction was developed to fit the differences observed in the named bands on the sarcomere at different degrees of muscle contraction and relaxation. The mechanism of contraction is the binding of myosin to actin, forming cross-bridges that generate filament movement (Figure 5).

Figure 5. When (a) a sarcomere (b) contracts, the Z lines move closer together and the I band gets smaller. The A band stays the same width and, at full contraction, the thin filaments overlap.
When a sarcomere shortens, some regions shorten whereas others stay the same length. A sarcomere is defined as the distance between two consecutive Z discs or Z lines; when a muscle contracts, the distance between the Z discs is reduced. The H zone—the central region of the A zone—contains only thick filaments (myosin) and is shortened during contraction. The H zone becomes smaller and smaller due to the increasing overlap of actin and myosin filaments, and the muscle shortens. Thus when the muscle is fully contracted, the H zone is no longer visible. The I band contains only thin filaments and also shortens. The A band does not shorten—it remains the same length—but A bands of different sarcomeres move closer together during contraction, eventually disappearing. Thin filaments are pulled by the thick filaments toward the center of the sarcomere until the Z discs approach the thick filaments. The zone of overlap, in which thin filaments and thick filaments occupy the same area, increases as the thin filaments move inward.
Note that the actin and myosin filaments themselves do not change length, but instead slide past each other.
ATP and Muscle Contraction
The motion of muscle shortening occurs as myosin heads bind to actin and pull the actin inwards. This action requires energy, which is provided by ATP. Myosin binds to actin at a binding site on the globular actin protein. Myosin has another binding site for ATP at which enzymatic activity hydrolyzes ATP to ADP, releasing an inorganic phosphate molecule and energy.
ATP binding causes myosin to release actin, allowing actin and myosin to detach from each other. After this happens, the newly bound ATP is converted to ADP and inorganic phosphate, Pi. The enzyme at the binding site on myosin is called ATPase. The energy released during ATP hydrolysis changes the angle of the myosin head into a “cocked” position. The myosin head is then in a position for further movement, possessing potential energy, but ADP and Pi are still attached. If actin binding sites are covered and unavailable, the myosin will remain in the high energy configuration with ATP hydrolyzed, but still attached.
If the actin binding sites are uncovered, a cross-bridge will form; that is, the myosin head spans the distance between the actin and myosin molecules. Pi is then released, allowing myosin to expend the stored energy as a conformational change. The myosin head moves toward the M line, pulling the actin along with it. As the actin is pulled, the filaments move approximately 10 nm toward the M line. This movement is called the power stroke, as it is the step at which force is produced. As the actin is pulled toward the M line, the sarcomere shortens and the muscle contracts.
When the myosin head is “cocked,” it contains energy and is in a high-energy configuration. This energy is expended as the myosin head moves through the power stroke; at the end of the power stroke, the myosin head is in a low-energy position. After the power stroke, ADP is released; however, the cross-bridge formed is still in place, and actin and myosin are bound together. ATP can then attach to myosin, which allows the cross-bridge cycle to start again and further muscle contraction can occur (Figure 6). The movement of the myosin head back to its original position is called the recovery stroke. Resting muscles store energy from ATP in the myosin heads while they wait for another contraction.

Figure 6. The cross-bridge muscle contraction cycle, which is triggered by Ca2+ binding to the actin active site, is shown. With each contraction cycle, actin moves relative to myosin.
Regulatory Proteins
When a muscle is in a resting state, actin and myosin are separated. To keep actin from binding to the active site on myosin, regulatory proteins block the molecular binding sites. Tropomyosin blocks myosin binding sites on actin molecules, preventing cross-bridge formation and preventing contraction in a muscle without nervous input. Troponin binds to tropomyosin and helps to position it on the actin molecule; it also binds calcium ions.
To enable a muscle contraction, tropomyosin must change conformation, uncovering the myosin-binding site on an actin molecule and allowing cross-bridge formation. This can only happen in the presence of calcium, which is kept at extremely low concentrations in the sarcoplasm. If present, calcium ions bind to troponin, causing conformational changes in troponin that allow tropomyosin to move away from the myosin binding sites on actin. Once the tropomyosin is removed, a cross-bridge can form between actin and myosin, triggering contraction. Cross-bridge cycling continues until Ca2+ ions and ATP are no longer available and tropomyosin again covers the binding sites on actin.
Watch this video explaining how a muscle contraction is signaled.
Practice Question
Which of the following statements about muscle contraction is true?
- The power stroke occurs when ATP is hydrolyzed to ADP and phosphate.
- The power stroke occurs when ADP and phosphate dissociate from the myosin head.
- The power stroke occurs when ADP and phosphate dissociate from the actin active site.
- The power stroke occurs when Ca2+ binds the calcium head.
Neural Stimulation of Muscle Contraction
The essence of the sliding filament model of muscle contraction is the action of actin and myosin sliding past each other. When this happens the sarcomere shortens and the muscle contracts. The process begins when a command or impulse is sent down a neuron that connects to muscle called a motor neuron.
The motor neuron releases a message in the form of a neurotransmitter to the muscle to tell it to contract. The neurotransmitter floats across an area between the neuron and muscle called the synaptic cleft. The muscle side of the synaptic cleft is called the motor end plate. The sarcolemma is enfolded at the motor end plate in order to increase the surface area. The neurotransmitter involved in skeletal muscle contraction is acetylcholine
Excitation–contraction coupling is the link (transduction) between the action potential generated in the sarcolemma and the start of a muscle contraction. The trigger for calcium release from the sarcoplasmic reticulum into the sarcoplasm is a neural signal. Each skeletal muscle fiber is controlled by a motor neuron, which conducts signals from the brain or spinal cord to the muscle. The area of the sarcolemma on the muscle fiber that interacts with the neuron is called the motor end plate. The end of the neuron’s axon is called the synaptic terminal, and it does not actually contact the motor end plate. A small space called the synaptic cleft separates the synaptic terminal from the motor end plate. Electrical signals travel along the neuron’s axon, which branches through the muscle and connects to individual muscle fibers at a neuromuscular junction.
The ability of cells to communicate electrically requires that the cells expend energy to create an electrical gradient across their cell membranes. This charge gradient is carried by ions, which are differentially distributed across the membrane. Each ion exerts an electrical influence and a concentration influence. Just as milk will eventually mix with coffee without the need to stir, ions also distribute themselves evenly, if they are permitted to do so. In this case, they are not permitted to return to an evenly mixed state.
The sodium–potassium ATPase uses cellular energy to move K+ ions inside the cell and Na+ ions outside. This alone accumulates a small electrical charge, but a big concentration gradient. There is lots of K+ in the cell and lots of Na+ outside the cell. Potassium is able to leave the cell through K+ channels that are open 90% of the time, and it does. However, Na+ channels are rarely open, so Na+remains outside the cell. When K+ leaves the cell, obeying its concentration gradient, that effectively leaves a negative charge behind. So at rest, there is a large concentration gradient for Na+ to enter the cell, and there is an accumulation of negative charges left behind in the cell. This is the resting membrane potential.
If an event changes the permeability of the membrane to Na+ ions, they will enter the cell. That will change the voltage. This is an electrical event, called an action potential, that can be used as a cellular signal. Communication occurs between nerves and muscles through neurotransmitters. Neuron action potentials cause the release of neurotransmitters from the synaptic terminal into the synaptic cleft, where they can then diffuse across the synaptic cleft and bind to a receptor molecule on the motor end plate. The motor end plate possesses junctional folds—folds in the sarcolemma that create a large surface area for the neurotransmitter to bind to receptors. The receptors are actually sodium channels that open to allow the passage of Na+ into the cell when they receive neurotransmitter signal.
Acetylcholine (ACh) is a neurotransmitter released by motor neurons that binds to receptors in the motor end plate. Neurotransmitter release occurs when an action potential travels down the motor neuron’s axon, resulting in altered permeability of the synaptic terminal membrane and an influx of calcium. The Ca2+ ions allow synaptic vesicles to move to and bind with the presynaptic membrane (on the neuron), and release neurotransmitter from the vesicles into the synaptic cleft. Once released by the synaptic terminal, ACh diffuses across the synaptic cleft to the motor end plate, where it binds with ACh receptors. As a neurotransmitter binds, these ion channels open, and Na+ ions cross the membrane into the muscle cell. This reduces the voltage difference between the inside and outside of the cell, which is called depolarization. As ACh binds at the motor end plate, this depolarization is called an end-plate potential. The depolarization then spreads along the sarcolemma, creating an action potential as sodium channels adjacent to the initial depolarization site sense the change in voltage and open. The action potential moves across the entire cell, creating a wave of depolarization.
ACh is broken down by the enzyme acetylcholinesterase (AChE) into acetyl and choline. AChE resides in the synaptic cleft, breaking down ACh so that it does not remain bound to ACh receptors, which would cause unwanted extended muscle contraction (Figure 7).
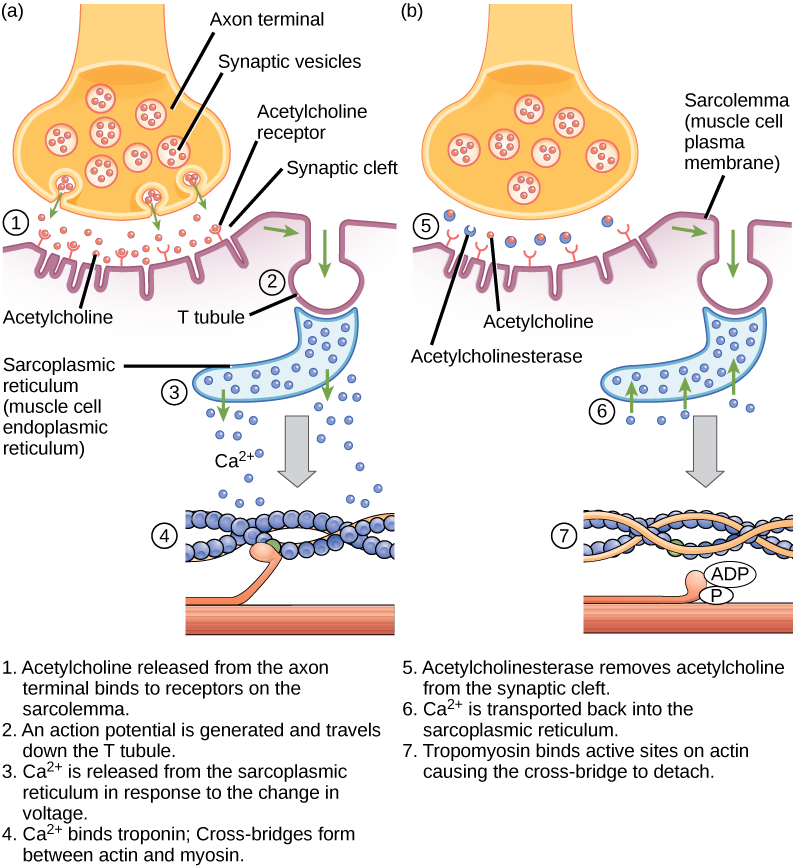
Figure 7. This diagram shows excitation-contraction coupling in a skeletal muscle contraction. The sarcoplasmic reticulum is a specialized endoplasmic reticulum found in muscle cells.
Practice Question
The deadly nerve gas Sarin irreversibly inhibits acetycholinesterase. What effect would Sarin have on muscle contraction?
Muscle Twitch and Control
Muscle Twitch
We can improve our understanding of muscle contraction by examining the contraction of one muscle fiber. A twitch occurs when one muscle fiber contracts in response to a command (stimulus) by the nervous system. The time between the activation of a motor neuron until the muscle contraction occurs is called the lag phase (sometimes called the latent phase). During the lag phase a signal called an action potential moves to the end of the motor neuron (axon terminal). This results in release of acetylcholine and depolarization of the motor end plate. The depolarization results in the release of calcium by the sarcoplasmic reticulum and subsequent binding of calcium to troponin which causes the myosin binding site to be exposes. This is followed by the actual muscle contraction that develops tension in the muscle. This next phase is called the contraction phase. During the contraction phase the cross-bridges between actin and myosin form. Myosin moves actin, releases and reforms cross-bridges many times as the sarcomere shortens and the muscle contracts. ATP is used during this phase and energy is released as heat. Myosin releases from actin when a second ATP attaches to myosin. Myosin is now available for another cross-bridge formation. When the muscle relaxes the tension decreases. This phase is called the relaxation phase. During this phase calcium is actively transported back into the sarcoplasmic reticulum using ATP. The troponin moves back into position blocking the myosin binding site on the actin and the muscle passively lengthens.
Muscle Stimulus and Contraction Strength
A skeletal muscle fiber will produce a given amount of force if the stimulus is strong enough to reach the threshold for muscle contraction. This is called the all or none law. Let’s say that we are electrically stimulating a muscle fiber. We begin with a low amount of stimulation that does not reach the threshold to produce a contraction. The muscle fiber will respond by remaining relaxed, it will not contract. Now if we increase the stimulation so that enough is produced to reach the threshold the muscle fiber will respond by contracting. Finally if we continue to increase the stimulus so that it well exceeds the threshold the fiber will respond by contracting with the same force as when we just reached the stimulus. The muscle will not contract with greater force if the stimulus is greater. The muscle responds to stronger stimuli by producing the same force. In skeletal muscles a motor neuron can innervate many muscle fibers. This is called a motor unit. There are numerous motor units throughout skeletal muscles. Motor units act in a coordinated fashion. One stimulus will affect all of the muscle fibers innervated by a given motor unit.
Muscle Length-Tension Relationship
Neural control initiates the formation of actin–myosin cross-bridges, leading to the sarcomere shortening involved in muscle contraction. These contractions extend from the muscle fiber through connective tissue to pull on bones, causing skeletal movement. The pull exerted by a muscle is called tension, and the amount of force created by this tension can vary. This enables the same muscles to move very light objects and very heavy objects. In individual muscle fibers, the amount of tension produced depends on the cross-sectional area of the muscle fiber and the frequency of neural stimulation.The length of a muscle is related to the tension generated by the muscle. Muscles will generate more force when stretched beyond their resting length to a point. Muscles stretched beyond this point will produce less tension. If the muscle is at its resting length it will not produce maximal tension because the actin and myosin filaments excessively overlap. Myosin filaments can extend into the Z-discs and both filaments interfere with each other limiting the number of cross-bridges that can form. If the muscle is stretched to a point the tension will increase in the muscle. The actin and myosin filaments can now optimally overlap so that the greatest number of cross-bridges can form. If the muscle is overstretched the tension will decrease. The actin and myosin filaments do not overlap causing a decrease in the number of cross-bridges that can form. The ideal length of a sarcomere during production of maximal tension occurs when thick and thin filaments overlap to the greatest degree.
Types of Muscle Fibers
There are three major types of skeletal muscle fibers. These are called fast twitch, slow twitch and intermediate. Generally, fast twitch fibers generate high force for brief periods of time. Slow twitch fibers generate lower amounts of force but can do so for longer periods of time. Intermediate fibers have some characteristics of both fast and slow twitch fibers. Fast twitch fibers are also called Type II fibers. Fast twitch fibers are the predominant fibers in the body. They respond quickly to stimuli and can generate a good deal of force. They have a large diameter due to the large amount of myofibrils. Their activity is fueled by ATP generated from anaerobic metabolism. Slow twitch fibers respond much more slowly to stimuli than fast twitch fibers. They are smaller in diameter and contain a large number of mitochondria. They are capable of sustaining long contractions and obtain their ATP from aerobic metabolism. Slow twitch fibers are surrounded by capillary networks that supply oxygenated blood for use in the aerobic energy systems. They also contain a red pigment called myoglobin. Myoglobin can bind oxygen (like hemoglobin) and provide a substantial oxygen reserve. Because of the reddish color of myoglobin these fibers are often called red muscle fibers. Slow twitch fibers are also called Type I fibers. Intermediate fibers resemble fast twitch fibers because they contain small amounts of myoglobin. They also have a capillary network around them and do not fatigue as readily as fast twitch fibers. They contain more mitochondria than fast twitch but not as many as slow twitch fibers. The speed of contraction and endurance also lie between fast and slow twitch fibers. Intermediate fibers are also called Type IIa fibers. Muscles that have a predominance of slow fibers are sometimes referred to as red muscles such as in the back and areas of the legs. Likewise muscles that have a predominance of fast fibers are referred to as white muscles. It is interesting to note that there are no slow twitch fibers in the eye muscles or muscles of the hands.
Muscles in Review
Muscle Physiology: The Big Picture
So how does a muscle contract?
In order to answer this question we must first examine what tells a muscle to contract. Let’s say that I am sitting here writing and want to pick up a cup of coffee. In order to do so I must send a command to the muscles in my arm. The command comes from a thought generated in my nervous system. The command travels from my brain to my spinal cord to a nerve that attaches to a muscle in my arm. The command tells my muscle to contract and my arm dutifully responds by moving closer to the coffee. Muscles are made of protein. If we were to examine a skeletal muscle under a microscope we would see that it is composed of tiny protein fibers or filaments. When a muscle receives a command from the nervous system to contract the protein filaments slide past each other. In fact one of the filaments connects to the other and drags it along. Think of thousands of overlapping filaments sliding past each other as the muscle contracts. The command to contract must somehow get from the outside of the muscle to the inside. Tiny messengers called neurotransmitters bring the message from the nerve to the muscle. Other chemical messengers that tell the protein filaments to contract then pass on the message. Muscles need energy to contract. Muscles must have some sort of power source in order to power the sliding filaments. The energy comes from ATP. ATP connects to one type of filament and extracts the energy so that it can pull the other filament along.
Skeletal Muscle Contractions
Steps of a skeletal muscle contraction:
- An action potential reaches the axon of the motor neuron.
- The action potential activates voltage gated calcium ion channels on the axon, and calcium rushes in.
- The calcium causes acetylcholine vesicles in the axon to fuse with the membrane, releasing the acetylcholine into the cleft between the axon and the motor end plate of the muscle fiber.
- The skeletal muscle fiber is excited by large mylenated nerve fibers which attach to the neuromuscular junction. There is one neuromuscular junction for each fiber.
- The acetylcholine diffuses across the cleft and binds to nicotinic receptors on the motor end plate, opening channels in the membrane for sodium and potassium. Sodium rushes in, and potassium rushes out. However, because sodium is more permeable, the muscle fiber membrane becomes more positively charged, triggering an action potential.
- The action potential on the muscle fiber causes the sarcoplasmic reticulum to release calcium ions(Ca++).
- The calcium binds to the troponin present on the thin filaments of the myofibrils. The troponin then allosterically modulates the tropomyosin. Normally the tropomyosin physically obstructs binding sites for cross-bridge; once calcium binds to the troponin, the troponin forces the tropomyosin to move out of the way, unblocking the binding sites.
- The cross-bridge (which is already in a ready-state) binds to the newly uncovered binding sites. It then delivers a power stroke.
- ATP binds the cross-bridge, forcing it to conform in such a way as to break the actin-myosin bond. Another ATP is split to energize the cross bridge again.
- Steps 7 and 8 repeat as long as calcium is present on thin filament.
- Throughout this process, the calcium is actively pumped back into the sarcoplasmic reticulum. When no longer present on the thin filament, the tropomyosin changes back to its previous state, so as to block the binding sites again. The cross-bridge then ceases binding to the thin filament, and the contractions cease as well.
- Muscle contraction remains as long as Ca+2 is abundant in sarcoplasm.
Types of Contractions
- Isometric contraction: muscle does not shorten during contraction and does not require the sliding of myofibrils but muscles are stiff.
- Isotonic contraction: inertia is used to move or work. More energy is used by the muscle and contraction lasts longer than isometric contraction. Isotonic muscle contraction is divided into two categories: concentric, where the muscle fibers shorten as the muscle contracts (ie. biceps brachialis on the up phase of a biceps curl); and eccentric, where the muscle fibers lengthen as they contract (ie. biceps brachialis on the down phase of a biceps curl).
- Twitch: exciting the nerve to a muscle or by passing electrical stimulus through muscle itself. Some fibers contract quickly while others contract slowly.
- Tonic: maintaining postural tone against the force of gravity.
Check Your Understanding
Answer the question(s) below to see how well you understand the topics covered in the previous section. This short quiz does not count toward your grade in the class, and you can retake it an unlimited number of times.
Use this quiz to check your understanding and decide whether to (1) study the previous section further or (2) move on to the next section.
Candela Citations
- Introduction to Muscle Contraction and Locomotion. Provided by: Lumen Learning. License: CC BY: Attribution
- Biology. Provided by: OpenStax CNX. Located at: http://cnx.org/contents/185cbf87-c72e-48f5-b51e-f14f21b5eabd@10.8. License: CC BY: Attribution. License Terms: Download for free at http://cnx.org/contents/185cbf87-c72e-48f5-b51e-f14f21b5eabd@10.8
- H Zone Diagram. Authored by: Bruce Forciea. Located at: http://www.bruceforciea.com/etextchapters/etexthumananatrevmay12.pdf. License: CC BY: Attribution
- Human Physiology. Provided by: Wikibooks. Located at: https://en.wikibooks.org/wiki/Human_Physiology. License: CC BY-SA: Attribution-ShareAlike
- An eText of Human Anatomy and Physiology. Authored by: Bruce Forciea. Located at: http://www.bruceforciea.com/etextchapters/etexthumananatrevmay12.pdf. License: CC BY: Attribution