Learning Objectives
- Interpret why certain disorders and diseases, such as gastroesophageal reflux disease (GERD), celiac disease, and irritable bowel syndrome compromise overall health.
When nutrients and energy are in short supply, cells, tissues, organs, and organ systems do not function properly. Unbalanced diets can cause diseases and, conversely, certain illnesses and diseases can cause an inadequate intake and absorption of nutrients, simulating the health consequences of an unbalanced diet. Overeating high-fat foods and nutrient-poor foods can lead to obesity and exacerbate the symptoms of gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS). Many diseases and illnesses, such as celiac disease, interfere with the body getting its nutritional requirements. A host of other conditions and illnesses, such as food allergies, cancer, stomach ulcers, Crohn’s disease, and kidney and liver disease, also can impair the process of digestion and/or negatively affect nutrient balance and decrease overall health.
Gastroesophageal Reflux Disease
Gastroesophageal reflux disease (GERD) is a persistent form of acid reflux that occurs more than two times per week. Acid reflux occurs when the acidic contents of the stomach leak backward into the esophagus and cause irritation. It is estimated that GERD affects 25 to 35 percent of the US population. An analysis of several studies published in the August 2005 issue of Annals of Internal Medicine concludes that GERD is much more prevalent in people who are obese.Hampel, H. MD, PhD, N. S. Abraham, MD, MSc(Epi) and H. B. El-Serag, MD, MPH. “Meta-Analysis: Obesity and the Risk for Gastroesophageal Reflux Disease and Its Complications.” Ann Intern Med 143, no. 3 (2005): 199–211. http://www.ncbi.nlm.nih.gov/pubmed/16061918 While the links between obesity and GERD are not completely known, they likely include that excess body fat puts pressure on the stomach, overeating increases pressure in the stomach, and fatty foods are triggers for GERD symptoms. The most common GERD symptom is heartburn, but people with GERD may also experience regurgitation (flow of the stomach’s acidic contents into the mouth), frequent coughing, and trouble swallowing. Approximately 35 percent of children born in the United States have GERD. In babies the symptoms are more difficult to distinguish from what babies do normally. The symptoms are spitting up more than normal, incessant crying, refusal to eat, burping, and coughing. Most babies outgrow GERD before their first birthday but a small percentage do not.
Heartburn is a burning sensation that radiates throughout the chest. © Shutterstock
Additional Facts about GERD
There are other causative factors of GERD that may be separate from or intertwined with obesity. The sphincter that separates the stomach’s internal contents from the esophagus often does not function properly and acidic gastric contents seep upward. Sometimes the peristaltic contractions of the esophagus are also sluggish and compromise the clearance of acidic contents. In addition to having an unbalanced, high-fat diet, some people with GERD are sensitive to particular foods—chocolate, garlic, spicy foods, fried foods, and tomato-based foods—which worsen symptoms. Drinks containing alcohol or caffeine may also worsen GERD symptoms. GERD is diagnosed most often by a history of the frequency of recurring symptoms. A more proper diagnosis can be made when a doctor inserts a small device into the lower esophagus that measures the acidity of the contents during one’s daily activities. Sometimes a doctor may use an endoscope, which is a long tube with a camera at the end, to view the tissue in the esophagus. About 50 percent of people with GERD have inflamed tissues in the esophagus. A condition known as Barrett’s esophagus may develop over time in some people who have GERD. Barrett’s esophagus refers to a structural difference in the tissue of the esophagus, which is caused by recurrent tissue damage. It occurs in 5 to 15 percent of patients diagnosed with GERD and less than 1 percent of these patients may develop cancer of the esophagus, a highly lethal cancer.
The first approach to GERD treatment is dietary and lifestyle modifications. Suggestions are to reduce weight if you are overweight or obese, avoid foods that worsen GERD symptoms, eat smaller meals, stop smoking, and remain upright for at least three hours after a meal. There is some evidence that sleeping on a bed with the head raised at least six inches helps lessen the symptoms of GERD. People with GERD may not take in the nutrients they need because of the pain and discomfort associated with eating. As a result, GERD can be caused by an unbalanced diet and its symptoms can lead to a worsening of nutrient inadequacy, a viscious cycle that further compromises health. Many medications are available to treat GERD, including antacids, histamine2 (H2) blockers, and proton-pump inhibitors. Some evidence from scientific studies indicates that medications used to treat GERD may accentuate certain nutrient deficiencies, namely zinc and magnesium. When these treatment approaches do not work surgery is an option. The most common surgery involves reinforcing the sphincter that serves as a barrier between the stomach and esophagus.
Irritable Bowel Syndome
Irritable bowel syndrome (IBS) is characterized by muscle spasms in the colon that result in abdominal pain, bloating, constipation, and/or diarrhea. Interestingly, IBS produces no permanent structural damage to the large intestine as often happens to patients who have Crohn’s disease or inflammatory bowel disease. It is estimated that one in five Americans displays symptoms of IBS. The disorder is more prevalent in women than men. Two primary factors that contribute to IBS are an unbalanced diet and stress. There is no specific test to diagnose IBS, but other conditions that have similar symptoms (such as celiac disease) must be ruled out. This involves stool tests, blood tests, and having a colonoscopy (which involves the insertion of a flexible tube with a tiny camera on the end through the anus so the doctor can see the colon tissues).
Symptoms of IBS significantly decrease a person’s quality of life as they are present for at least twelve consecutive or nonconsecutive weeks in a year. Large meals and foods high in fat and added sugars, or those that contain wheat, rye, barley, peppermint, and chocolate intensify or bring about symptoms of IBS. Additionally, beverages containing caffeine or alcohol may worsen IBS. Stress and depression compound the severity and frequency of IBS symptoms. As with GERD, the first treatment approaches for IBS are diet and lifestyle modifications. People with IBS are often told to keep a daily food journal to help identify and eliminate foods that cause the most problems. Other recommendations are to eat slower, add more fiber to the diet, drink more water, and to exercise. There are some medications (many of which can be purchased over-the-counter) to treat IBS and the resulting diarrhea or constipation. Sometimes antidepressants and drugs to relax the colon are prescribed.
Celiac Disease
Celiac disease is an autoimmune disorder affecting between 0.5 and 1.0 percent of Americans—that is, one in every one- to two-hundred people. It is caused by an abnormal immune reaction of small intestine cells to a type of protein, called gluten. Gluten forms in the presence of water and is composed of two protein parts, glutenin and gliadin. Glutenin and gliadin are found in grains that are commonly used to make bread, such as wheat, rye, and barley. When bread is made, yeast eats the flour and makes a waste product, carbon dioxide, which forms bubbles in the dough. As the dough is kneaded, gluten forms and stretches. The carbon dioxide gas bubbles infiltrate the stretchy gluten, giving bread its porosity and tenderness. For those who are sensitive to gluten, it is good to know that corn, millet, buckwheat, and oats do not contain the proteins that make gluten. However, some people who have celiac disease also may have a response to products containing oats. This is most likely the result of cross-contamination of grains during harvest, storage, packaging, and processing.
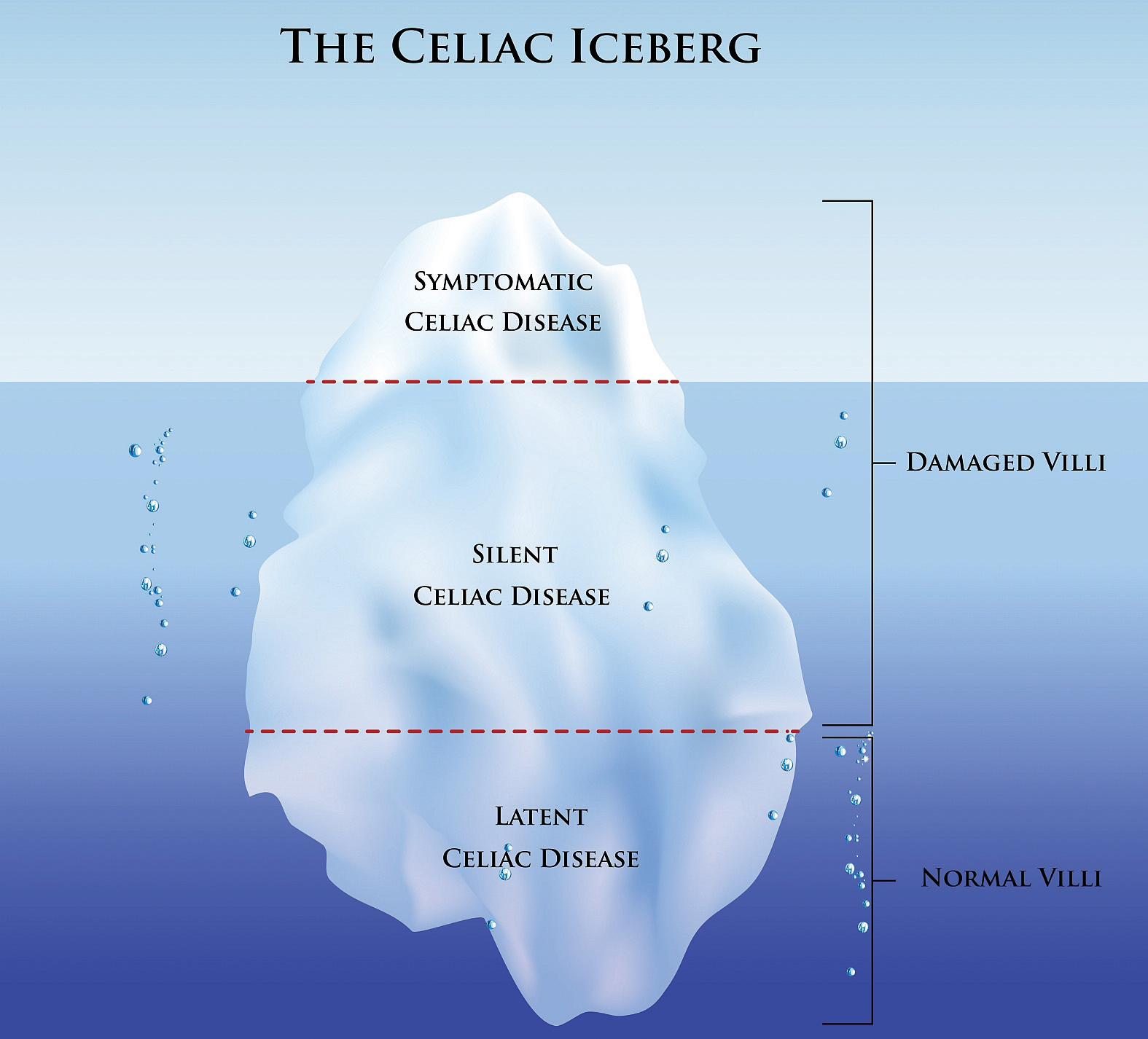
Figure 3.6.1: Celiac: Not everyone with celiac is diagnosed—many have “silent” or “latent” celiac disease. © Shutterstock
Celiac disease is most common in people of European descent and is rare in people of African American, Japanese, and Chinese descent. It is much more prevalent in women and in people with Type 1 diabetes, autoimmune thyroid disease, and Down and Turner syndromes. Symptoms can range from mild to severe and can include pale, fatty, loose stools, gastrointestinal upset, abdominal pain, weight loss and, in children, a failure to grow and thrive. The symptoms can appear in infancy or much later in life, even by age seventy. Celiac disease is not always diagnosed because the symptoms may be mild. A large number of people have what is referred to as “silent” or “latent” celiac disease (Figure 3.6.1).
Celiac disease diagnosis requires a blood test and a biopsy of the small intestine. Because celiac disease is an autoimmune disease, antibodies produced by white blood cells circulate in the body and can be detected in the blood. When gluten-containing foods are consumed the antibodies attack cells lining the small intestine leading to a destruction of the small villi projections. This tissue damage can be detected with a biopsy, a procedure that removes a portion of tissue from the damaged organ. Villi destruction is what causes many of the symptoms of celiac disease. The destruction of the absorptive surface of the small intestine also results in the malabsorption of nutrients, so that while people with this disease may eat enough, nutrients do not make it to the bloodstream because absorption is reduced. The effects of nutrient malabsorption are most apparent in children and the elderly as they are especially susceptible to nutrient deficiencies. Over time these nutrient deficiencies can cause health problems. Poor absorption of iron and folic acid can cause anemia, which is a decrease in red blood cells. Anemia impairs oxygen transport to all cells in the body. Calcium and vitamin D deficiences can lead to osteoporosis, a disease in which bones become brittle.
If you think you or someone close to you may have celiac disease, do not despair; it is a very treatable disease. Once diagnosed, a person follows a gluten-free diet for life. This requires dedication and careful detective work to seek out foods with hidden gluten, but some stores carry gluten-free foods. After eliminating gluten from the diet, the tissues of the small intestine rapidly repair themselves and heal in less than six months.
Food Allergies
Paying attention to the way individuals react to various foods is essential in determining what foods may specifically affect a person adversely. Food allergies are one of the many ways in which different body make-ups affect nutritional concerns. Although an estimated twelve million Americans have food allergies, there are likely many more people who say they have food allergies than actually do. This is because food sensitization is different from a medically-determined food allergy. When someone has a food allergy, the immune system mistakenly attacks a certain kind of food (usually the protein component of a food), such as peanuts, as if it were a threat and IgE antibodies are produced. Doctors sometimes test for food allergies by using skin-prick tests or blood tests to look for the presence of IgE antibodies. However, these types of tests are not always reliable as they can sometimes yield a false positive result. By far, the most valuable tests for determining a food allergy is the Double Blind Placebo Controlled Food Challenge (DBPCFC), which involves administering the food orally and then denoting the signs and symptoms of the allergic response.

Many people with food allergies experience skin rashes after eating an allergenic food. © Shutterstock
Food allergy symptoms usually develop within a few minutes to two hours after a person has eaten a food to which they are allergic. These symptoms can range from the annoying to the potentially fatal, and include:
- A tingling mouth
- Swelling tongue and/or throat
- Difficulty breathing
- Hives
- Stomach cramps
- Diarrhea
- Vomiting
- Drop in blood pressure
- Loss of consciousness
- Death
There are no clear treatments for food allergies. Epinephrine is sometimes used to control severe reactions, and individuals with known and dangerous allergies may get prescriptions for self-injectable devices. The only certain way to avoid allergic reactions to food is to avoid the foods that cause them. Beyond avoidance, this can mean reading food labels carefully, or even calling manufacturers for product information.
Ninety percent of food allergies are caused by these eight foods:
- Milk
- Eggs
- Peanuts
- Tree nuts
- Fish
- Shellfish
- Wheat
- Soy
The prevalence of food allergies is a complex and growing problem. In response to this situation, the National Institute of Allergy and Infectious Diseases (NIAID) collaborated with thirty-four professional organizations, federal agencies, and patient-advocacy groups to develop a comprehensive guide to diagnosing and managing food allergies and treating acute food allergy reactions. The guide defines various food allergies, allergens, and reactions, provides comprehensive information on the prevalence of different food allergies, tracks the history of food allergies, and reviews medical management techniques for people with food allergies.
Key Takeaways
- Unbalanced diets can cause diseases and, conversely, certain disorders and diseases can cause an inadequate intake and absorption of nutrients simulating the health consequences of an unbalanced diet.
- Unbalanced, high-fat diets can exacerbate the symptoms of GERD and IBS.
- Celiac disease and anorexia can lead to nutritional deficiencies, which compromise functioning of the organ systems and decrease health.
- Food allergies affect roughly twelve million Americans, with symptoms that range from mild to deadly. Proper diagnosis leads to better management of food allergies and sensitivities.
Discussion Starter
- The next time you visit the grocery store, be a “gluten detective” and use the ingredients list to identify all the foods you might normally purchase that contain gluten. Discuss how you can use food labels to avoid products containing gluten.
Candela Citations
- Disorders That Can Compromise Health. Authored by: Medical LibreTexts Contributors. Provided by: LibreTexts. Located at: https://med.libretexts.org/Courses/Sacramento_City_College/SCC%3A_Nutri_300_(Coppola)/Chapters/03%3A_Nutrition_and_the_Human_Body/3.6%3A_Disorders_That_Can_Compromise_Health. License: CC BY-NC-SA: Attribution-NonCommercial-ShareAlike
