Learning Objectives
- Explain forensic issues in psychological treatment, such as the insanity defense, competency to stand trial, and understanding the purpose of punishment

Figure 1. Jared Lee Loughner, a convicted mass murderer, was originally ruled incompetent to stand trial due to a diagnosis of paranoid schizophrenia but was later ruled competent and sentenced to life plus 140 years in federal prison.
Jared Lee Loughner (born September 10, 1988) is a convicted American mass murderer who pled guilty to 19 charges of murder and attempted murder in connection with the January 8, 2011, Tucson shooting. After his arrest, two medical evaluations diagnosed Loughner with paranoid schizophrenia and ruled him incompetent to stand trial. Punishment or treatment? What should we do when someone who is mentally ill but commits a horrendous crime?
In this section, we will discuss the forensic issues in psychological treatment, such as the insanity defense, competency to stand trial, and the purpose of punishment. We will also examine the ethical and legal issues in providing service and the rights of mentally ill patients. What is the legal responsibility or duty of mental health care providers to protect individuals who are being threatened with bodily harm by a patient in their care. Should we honor the right to refuse treatment when someone is psychologically disturbed? Should psychiatrists administer antipsychotics or any other drug deemed necessary to treat patients against their will? Should mentally ill clients with a history of violent behavior be recommended for commitment or involuntary hospitalization? How do we balance the rights of the individual with the rights of society? Does the answer to these questions lie with the criminal justice system or with the mental health system?
Below, we begin by summarizing the major perspectives on ethical and forensic issues in psychological treatment.
Tarasoff v. Regents of the University of California
Tarasoff v. Regents of the University of California, (Cal. 1976), was a case in which the Supreme Court of California held that mental health professionals have a duty to protect individuals who are being threatened with bodily harm by a patient. The original 1974 decision mandated warning the threatened individual, but a 1976 rehearing of the case by the California Supreme Court called for a “duty to protect” the intended victim. The professional may discharge the duty in several ways, including notifying police, warning the intended victim, and/or taking other reasonable steps to protect the threatened individual.
History
Prosenjit Poddar was a student from Bengal, India. He entered the University of California, Berkeley, as a graduate student in September 1967 and resided at International House. In the fall of 1968, he attended folk dancing classes at the International House, and it was there that he met Tatiana Tarasoff. They dated, but apparently had different ideas about the relationship. He assumed their relationship was serious. This view was not shared by Tarasoff who, upon learning of his feelings, told him that she was involved with other men and that she was not interested in entering into an intimate relationship with him. This statement gave rise to feelings of resentment in Poddar. He began to stalk her.
After this rebuff, Poddar underwent a severe emotional crisis. He became depressed and neglected his appearance, his studies, and his health. He kept to himself, speaking disjointedly and often weeping. This condition persisted, with steady deterioration, throughout the spring and into the summer of 1969. Poddar had occasional meetings with Tarasoff during this period and tape-recorded their various conversations to try to find out why she did not love him.
During the summer of 1969, Tarasoff went to South America. After her departure, Poddar began to improve and at the suggestion of a friend sought psychological assistance. Prosenjit Poddar was a patient of Dr. Lawrence Moore, a psychologist at UC Berkeley’s Cowell Memorial Hospital in 1969. Poddar confided his intent to kill Tarasoff. Dr. Moore requested that the campus police detain Poddar, writing that, in his opinion, Poddar was suffering from paranoid schizophrenia, acute and severe. The psychologist recommended that the defendant be civilly committed as a dangerous person. Poddar was detained but shortly thereafter released, as he appeared rational. Dr. Moore’s supervisor, Dr. Harvey Powelson, then ordered that Poddar not be subject to further detention.
In October, after Tarasoff had returned, Poddar stopped seeing his psychologist. Neither Tarasoff nor her parents received any warning of the threat. Poddar then befriended Tarasoff’s brother, even moving in with him. Several weeks later, on October 27, 1969, Poddar carried out the plan he had confided to his psychologist, stabbing and killing Tarasoff. Tarasoff’s parents then sued Moore and various other employees of the university.
Poddar was subsequently convicted of second-degree murder, but the conviction was later appealed and overturned on the grounds that the jury was inadequately instructed. A second trial was not held, and Poddar was released on the condition that he would return to India.
Opinion of the court
The California Supreme Court found that a mental health professional has a duty not only to a patient, but also to individuals who are specifically being threatened by a patient. This decision has since been adopted by most states in the United States and is widely influential in jurisdictions outside the United States as well.
Subsequent developments
As of 2012, a duty to warn or protect is mandated and codified in legislative statutes of 23 states, while the duty is not codified in a statute but is present in the common law supported by precedent in 10 states. Eleven states have a permissive duty, and six states are described as having no statutes or case law offering guidance.
In 2018, the Court held that universities should protect students in the Regents of University of California v. Superior Court of Los Angeles County.
Commitment of Clients
Starting in the 1960s, there has been a worldwide trend toward moving psychiatric patients from hospital settings to less restricting settings in the community, a shift known as “deinstitutionalization.” Because the shift was typically not accompanied by a commensurate development of community-based services, critics say that deinstitutionalization has led to large numbers of people who would once have been inpatients as instead being incarcerated or becoming homeless. In some jurisdictions, laws authorizing court-ordered outpatient treatment have been passed in an effort to compel individuals with chronic, untreated, severe mental illness to take psychiatric medication while living outside the hospital (see Laura’s Law, Kendra’s Law).
In most jurisdictions, involuntary commitment is applied to individuals believed to be experiencing a mental illness that impairs their ability to reason to such an extent that the agents of the law, state, or courts determine that decisions will be made for the individual under a legal framework. This is a proceeding distinct from being found incompetent and limits involuntary treatment to individuals who meet statutory criteria for presenting a danger to self or others. Involuntary commitment is a legal process through which an individual who is deemed by a qualified agent to have symptoms of severe mental disorder is detained in a psychiatric hospital (inpatient) where they can be treated involuntarily. This treatment may involve the administration of psychoactive drugs including involuntary administration. In many jurisdictions, people diagnosed with mental health disorders can also be forced to undergo treatment while in the community, this is sometimes referred to as outpatient commitment and shares legal processes with commitment.
A number of civil and human rights activists, anti-psychiatry groups, medical and academic organizations, researchers, and members of the psychiatric survivors movement vigorously oppose involuntary treatment on human rights grounds or on grounds of effectiveness and medical appropriateness, particularly with respect to involuntary administration of mind-altering substances, ECT, and psycho-surgery. Some criticism has been made regarding cost, as well as of conflicts of interest with the pharmaceutical industry. Critics, such as the New York Civil Liberties Union, have denounced the strong racial and socioeconomic biases in forced treatment orders. Supporters of involuntary treatment include organizations such as the National Alliance on Mental Illness (NAMI) and the American Psychiatric Association.
Right to treatment and Refusal of Treatment
In October 1970, Ricky Wyatt was a fifteen-year-old who had always been labeled a “juvenile delinquent.” Despite not being indicated with a mental illness, he was a patient at Bryce Hospital (first known as the Alabama State Hospital for the Insane) and became the named plaintiff in a landmark class-action lawsuit, Wyatt v. Stickney. His aunt, W. C. Rawlins, was one of the employees at Bryce who had been laid off. Together they testified about intolerable conditions and improper treatments designed only to make the patients more manageable. In 1971, the plaintiff class was expanded to include patients at Alabama’s two other inpatient mental health facilities. The right to treatment emerged as the outcome and resulted in federal minimum standards for the care of people with mental illness or mental retardation who reside in institutional settings.
The standards elaborated in that agreement have served as a model nationwide. Known as the “Wyatt Standards,” they are founded on four criteria for evaluation of care:
- humane psychological and physical environment
- qualified and sufficient staff for administration of treatment
- individualized treatment plans
- minimum restriction of patient freedom.
The case of Wyatt v. Stickney came to a conclusion after 33 years, through the tenure of nine Alabama governors and fourteen state mental health commissioners, the longest mental health case in national history. The State of Alabama estimates its litigation expenses at over $15 million.
Just as clients have a right to treatment, they also have a right to refuse unwanted treatment. Informed refusal is where a person has refused a recommended medical treatment based on an understanding of the facts and the implications of not following the treatment. Informed refusal is linked to the informed consent process, as a patient has a right to consent, but also may choose to refuse.
The individual needs to be in possession of the relevant facts as well as of their reasoning faculties, such as not being intellectually disabled or mentally ill and without impairment of judgment at the time of refusing. In cases where an individual is considered unable to give informed refusal, another person (a guardian) may be authorized to give consent on their behalf. Substituted judgment generally is a decision made by a person on behalf of a person who is incompetent and unable to decide for himself or herself. Substituted judgment with regard to guardianship is the standard that directs the decision making of a guardian.
When refusal of treatment may result in significant damage or death, the interaction needs to be documented to protect the care giver in a potential later litigation against the allegation that the recommendation was either not made or not understood. On occasion, a patient will also refuse to sign the “informed refusal” document, in which case a witness would have to sign that the informed process and the refusal took place. The pregnant patient represents a specific dilemma in the field of informed refusal as her action may result in harm or death to the fetus. Ethicists disagree on how to handle this situation.
Clients also have the right for placement in a least restrictive alternative to treatment in an institution. O’Connor v. Donaldson, 422 U.S. 563 (1975), was a landmark decision of the U.S. Supreme Court in mental health law ruling that a state cannot constitutionally confine a non-dangerous individual who is capable of surviving safely in freedom by themselves or with the help of willing and responsible family members or friends. Kenneth Donaldson (confined patient diagnosed with paranoid schizophrenia and civilly committed) had been held for 15 years in Florida State Hospital at Chattahoochee, due to needs of “care, maintenance, and treatment.” He filed a lawsuit against the hospital and staff members claiming they had robbed him of his constitutional rights, by confining him against his will. Donaldson won his case since the trial court jury found, upon ample evidence, that the petitioner had violated Donaldson’s right to liberty. A finding of mental illness alone cannot justify a State’s locking a person up against his will and keeping him indefinitely in simple custodial confinement. Assuming that that term can be given a reasonably precise content and that the mentally ill can be identified with reasonable accuracy, there is still no constitutional basis for confining such persons involuntarily if they are dangerous to no one and can live safely in freedom.
The Insanity Defense
The insanity defense is an affirmative defense by excuse in a criminal case, arguing that the defendant is not responsible for their actions due to an episodic or persistent psychiatric disorder at the time of the criminal act. Legal definitions of insanity or mental disorder are varied, and include the M’Naghten Rule, the Durham rule, the ALI rule (American Legal Institute Model Penal Code rule), and other provisions, often relating to a lack of mens rea (“guilty mind”).
Being incapable of distinguishing right from wrong is one basis for being found to be legally insane as a criminal defense. It originated in the M’Naghten Rule, formulated as a reaction to the acquittal in 1843 of Daniel M’Naghten, a Scottish woodturner who assassinated an English civil servant while suffering from paranoid delusions. M’Naghten had mistaken him as the UK Prime Minister, the intended target, and believed he was following the commands of a higher power. The central issue of the M’Naghten Rules may be stated as, “did the defendant know what they were doing, or, if so, that it was wrong?”
Legislators added the irresistible impulse defense, in which the defendant argues that they should not be held criminally liable for their actions that broke the law, because they could not control those actions, even if they knew them to be wrong. In 1994, Lorena Bobbitt was found not guilty when her defense argued that an irresistible impulse led her to cut off her husband’s penis with a knife while he was asleep in bed. The husband-wife relationship made world-wide headlines in 1993 and revealed that Lorena has been subjected to years of being raped, beaten, and sodomized by her husband. It is a variant of the M’Naghten Rules that addresses the situation in which defendants knew that what they were going to do was wrong, but had no ability to restrain themselves from doing it.
The Durham rule later expanded the insanity defense and established that a jury may determine a defendant is not guilty by reason of insanity because the criminal act was the product of a mental disorder. Examples in which such rules were articulated State v. Pike (1869) and Durham v. United States (1954). After the 1970s, U.S. jurisdictions have tended to not recognize this argument as it places emphasis on “mental disease or defect” and thus on testimony by psychiatrists and is argued to be somewhat ambiguous. It gave psychiatric and psychological experts too much influence in a decision of insanity and not enough to jurors.
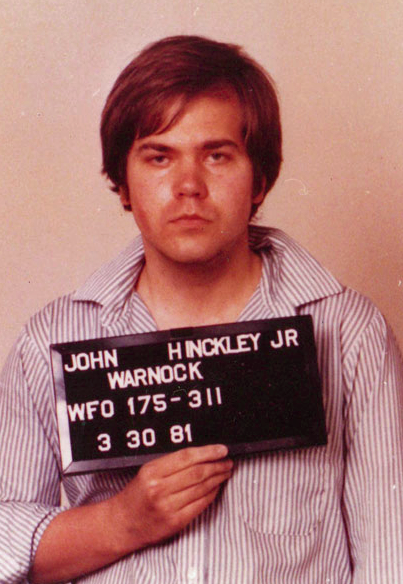
Figure 2. On March 30, 1981, United States President Ronald Reagan was shot and wounded by John Hinckley Jr. in Washington, D.C. as he was returning to his limousine after a speaking engagement at the Washington Hilton Hotel. Hinckley believed the attack would impress actress Jodie Foster, with whom he had become obsessed.
The ALI rule, or American Law Institute Model Penal Code rule, is a recommended rule for instructing juries how to find a defendant in a criminal trial is not guilty by reason of insanity. It broadened the M’Naghten rule. It arose from the case of United States v. Brawner. The case overturned the Durham rule ( that put substantial dominance on the testimony of experts) gave jurers a specific framework for the insanity defense. The focus is on the acts and mental state of a defendant at the time he committed the acts constituting the crime.
- The ALI rule is:
- “(1) A person is not responsible for criminal conduct if at the time of such conduct as a result of mental disease of defect he lacks substantial capacity either to appreciate the criminality of his conduct or to conform his conduct to the requirements of the law.
- “(2) As used in this Article, the terms “mental disease or defect” do not include an abnormality manifested only by repeated criminal or otherwise antisocial conduct [Section 4.01].”[1]
John Hinckley, Jr. is an American who, on March 30, 1981, attempted to assassinate U.S. President Ronald Reagan in Washington, D.C. He wounded Reagan with a bullet from a revolver that ricocheted and hit Reagan in the chest. He also wounded police officer Thomas Delahanty and Secret Service agent Tim McCarthy, and he critically wounded Press Secretary James Brady, who was permanently disabled in the shooting and later died from those injuries. Hinckley was reportedly seeking fame in order to impress actress Jodie Foster, on whom he had an obsessive fixation. He was found not guilty by reason of insanity and remained under institutional psychiatric care until September 10, 2016. Public outcry over the verdict led to the Insanity Defense Reform Act of 1984, which altered the rules for consideration of mental illness of defendants in Federal Criminal Court proceedings in the United States. In January 2015, federal prosecutors announced that they would not charge Hinckley with Brady’s death, despite the medical examiner’s classification of his death as a homicide. Along with Lynette Fromme and Sara Jane Moore, Hinckley is one of three attempted presidential assassins currently living who are not in prison. Hinckley is portrayed by Steven Flynn in the American television film, Without Warning: The James Brady Story (1991).
Competence to Stand Trial
The word incompetent is used to describe persons who should not undergo or partake in certain judicial processes, and also for those who lack the mental capacity to make contracts, handle their financial and other personal matters such as consenting to medical treatment, etc. and need a legal guardian to handle their affairs. When it comes to competence to stand trial and the law, the right to not be prosecuted while one is incompetent to stand trial has been ruled by the United States Supreme Court to be guaranteed under the due process clause, which acts as a safeguard from arbitrary denial of life, liberty, or property by the government outside the sanction of law. Dusky v. United States, (1960), was a landmark United States Supreme Court case in which the Court affirmed a defendant’s right to have a competency evaluation before proceeding to trial.
If the court determines that a defendant’s mental condition makes him unable to understand the proceedings, or that he is unable to help in his defense, he is found incompetent. Being determined incompetent is substantially different from undertaking an insanity defense; competence regards the defendant’s state of mind at the time of the trial, while insanity regards his state of mind at the time of the crime. A ruling of incompetence may later be reversed. A defendant may recover from a mental illness or disability, and a court may require a defendant to undergo treatment in an effort to render the defendant competent to stand trial. For example, in 1989, Kenneth L. Curtis of Stratford, Connecticut, was found mentally incompetent to stand trial following the murder of his estranged girlfriend. But years later, as he had attended college and received good grades, this ruling was reversed, and he was ordered to stand trial.
Understanding the Purpose of Punishment
Is a mentally ill person convicted of a capital offense able or competent enough to understand the nature and purpose of the death sentence? The case of Alvin Bernard Ford highlights the complexity of the issue. Ford v. Wainwright, 477 U.S. 399 (1986), was a landmark case that upheld the common law rule that the insane cannot be executed. Ford was convicted of murder in 1974 and sentenced to death in Florida. In 1982, while on death row, Ford’s mental health diminished to a point resembling paranoid schizophrenia. Ford began referring to himself as Pope John Paul III and reported such accomplishments as thwarting a vast Ku Klux Klan conspiracy to bury dead prisoners inside the prison walls, foiling an attempt by prison guards to torture his female relatives inside the prison, and personally appointing nine new justices to the Florida Supreme Court. A panel of three psychiatrists was eventually called to examine Ford’s behavior, and it concluded that while Ford suffered from psychosis and various mental disorders, he was still capable of understanding the nature of the death penalty and the effect that such a penalty would have on him. A death warrant was signed for Ford in 1984. Ford sued the secretary of the Florida Department of Corrections, Louie L. Wainwright, and took his case to the United States Supreme Court, declaring he was not competent to be executed. The court ruled in his favor, then further addressed the procedural issues present in making a determination of insanity for Eighth Amendment concerns (cruel and unusual punishment). The Court, in an opinion by Justice Marshall, reviewed the evolving standards of the Eighth Amendment to be those consistent with “the progress of a maturing society,” and one not tolerable of acts traditionally branded as “savage and inhumane,” as the execution of the mentally insane. The inmate was transferred to Florida State Hospital for treatment after he was reevaluated and found to be incompetent to be executed. In 1989, a federal district judge ruled that Ford was sane, but defense lawyers appealed that ruling. The appeal was pending when Ford died on February 6, 1991 of natural causes, at 37.
Today, an inmate on death row has a right to be evaluated for competency by a forensic expert to determine if the sentence can be carried out. If the inmate is found incompetent, a forensic professional must provide treatment to aid in his gaining competency so the execution can take place.
Try It
glossary
ALI rule: a recommended rule for instructing juries how to find a defendant in a criminal trial is not guilty by reason of insanity; the focus is on the acts and mental state of a defendant at the time he committed the acts constituting the crime
competence to stand trial: the right to not be prosecuted while one is incompetent to stand trial
Durham rule: established that a jury may determine a defendant is not guilty by reason of insanity because the criminal act was the product of a mental disorder
duty to warn or protect: holds that mental health professionals have a duty to protect individuals who are being threatened with bodily harm by a patient
guardian: a person authorized to give consent on behalf of a person who is unable to decide for himself or herself
incompetent: used to describe persons who should not undergo or partake in certain judicial processes, and also for those who lack mental capacity to make contracts, handle their financial and other personal matters such as consenting to medical treatment, etc., and need a legal guardian to handle their affairs
insanity defense: an affirmative defense by excuse in a criminal case, arguing that the defendant is not responsible for their actions due to an episodic or persistent psychiatric disorder at the time of the criminal act
involuntary commitment: civil commitment or involuntary hospitalization—a legal process through which an individual who is deemed by a qualified agent to have symptoms of severe mental disorder is detained in a psychiatric hospital (inpatient) where they can be treated involuntarily
irresistible impulse: defense in which the defendant argues that they should not be held criminally liable for their actions that broke the law because they could not control those actions, even if they knew them to be wrong
least restrictive alternative: law ruling that a state cannot constitutionally confine a non-dangerous individual who is capable of surviving safely in freedom
right to treatment: federal minimum standards for the care of people with mental illness or mental retardation who reside in institutional settings
substituted judgment: a decision made by a person on behalf of a person who is incompetent and unable to decide for himself or herself
Candela Citations
- Modification, adaptation, and original content. Authored by: Sonja Ann Miller for Lumen Learning. Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike
- Tarasoff v. Regents of the University of California. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Tarasoff_v._Regents_of_the_University_of_California. License: CC BY-SA: Attribution-ShareAlike
- Jared Lee Loughner. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Jared_Lee_Loughner. License: CC BY-SA: Attribution-ShareAlike
- Involuntary commitment. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Involuntary_commitment. License: CC BY-SA: Attribution-ShareAlike
- Involuntary_treatment. Located at: https://en.wikipedia.org/wiki/Involuntary_treatment. License: CC BY-SA: Attribution-ShareAlike
- Bryce Hospital. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Bryce_Hospital#Wyatt_v._Stickney. License: CC BY-SA: Attribution-ShareAlike
- Informed refusal. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Informed_refusal. License: CC BY-SA: Attribution-ShareAlike
- O'Connor v. Donaldson. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/O%27Connor_v._Donaldson. License: CC BY-SA: Attribution-ShareAlike
- Insanity defense. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Insanity_defense. License: CC BY-SA: Attribution-ShareAlike
- Daniel M'Naghten. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Daniel_M%27Naghten. License: CC BY-SA: Attribution-ShareAlike
- Irresistible impulse. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Irresistible_impulse. License: CC BY-SA: Attribution-ShareAlike
- John and Lorena Bobbitt. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/John_and_Lorena_Bobbitt. License: CC BY-SA: Attribution-ShareAlike
- Durham rule. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Durham_rule. License: CC BY-SA: Attribution-ShareAlike
- United States v. Brawner. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/United_States_v._Brawner. License: CC BY-SA: Attribution-ShareAlike
- ALI Rule. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/ALI_rule. License: CC BY-ND: Attribution-NoDerivatives
- Attempted assassination of Ronald Reagan. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Attempted_assassination_of_Ronald_Reagan. License: CC BY-SA: Attribution-ShareAlike
- John Hinckley Jr.. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/John_Hinckley_Jr.. License: CC BY-SA: Attribution-ShareAlike
- Due Process Clause. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Due_Process_Clause. License: CC BY-SA: Attribution-ShareAlike
- Competence (law). Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Competence_(law)#Competence_to_stand_trial. License: CC BY-SA: Attribution-ShareAlike
- Dusky v. United_States. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Dusky_v._United_States. License: CC BY-SA: Attribution-ShareAlike
- Ford v. Wainwright. Provided by: Wikipedia. Located at: https://en.wikipedia.org/wiki/Ford_v._Wainwright. License: CC BY-SA: Attribution-ShareAlike
- Loughner mugshot. Provided by: Wikimedia. Located at: https://en.wikipedia.org/wiki/Jared_Lee_Loughner. License: Public Domain: No Known Copyright
- Criminal Law—Cases and Materials, 7th ed. 2012, Wolters Kluwer Law & Business; John Kaplan, Robert Weisberg, Guyora Binder, ISBN 978-1-4548-0698-1 ↵
