Somatosensation
Somatosensation is considered a general sense, as opposed to the special senses discussed in this section. Somatosensation is the group of sensory modalities that are associated with touch, proprioception, and interoception. These modalities include pressure, vibration, light touch, tickle, itch, temperature, pain, proprioception, and kinesthesia. This means that its receptors are not associated with a specialized organ, but are instead spread throughout the body in a variety of organs. Many of the somatosensory receptors are located in the skin, but receptors are also found in muscles, tendons, joint capsules, ligaments, and in the walls of visceral organs. Two types of somatosensory signals that are transduced by free nerve endings are pain and temperature. These two modalities use thermoreceptors and nociceptors to transduce temperature and pain stimuli, respectively. Temperature receptors are stimulated when local temperatures differ from body temperature.
Some thermoreceptors are sensitive to just cold and others to just heat. Nociception is the sensation of potentially damaging stimuli. Mechanical, chemical, or thermal stimuli beyond a set threshold will elicit painful sensations. Stressed or damaged tissues release chemicals that activate receptor proteins in the nociceptors.
For example, the sensation of heat associated with spicy foods involves capsaicin, the active molecule in hot peppers. Capsaicin molecules bind to a transmembrane ion channel in nociceptors that is sensitive to temperatures above 37°C. The dynamics of capsaicin binding with this transmembrane ion channel is unusual in that the molecule remains bound for a long time. Because of this, it will decrease the ability of other stimuli to elicit pain sensations through the activated nociceptor. For this reason, capsaicin can be used as a topical analgesic, such as in products such as Icy Hot™.
If you drag your finger across a textured surface, the skin of your finger will vibrate. Such low frequency vibrations are sensed by mechanoreceptors called Merkel cells, also known as type I cutaneous mechanoreceptors. Merkel cells are located in the stratum basale of the epidermis (Figure 1). Deep pressure and vibration is transduced by lamellated (Pacinian) corpuscles, which are receptors with encapsulated endings found deep in the dermis, or subcutaneous tissue. Light touch is transduced by the encapsulated endings known as tactile (Meissner) corpuscles. Follicles are also wrapped in a plexus of nerve endings known as the hair follicle plexus. These nerve endings detect the movement of hair at the surface of the skin, such as when an insect may be walking along the skin. Stretching of the skin is transduced by stretch receptors known as bulbous corpuscles. Bulbous corpuscles are also known as Ruffini corpuscles, or type II cutaneous mechanoreceptors.
Other somatosensory receptors are found in the joints and muscles. Stretch receptors monitor the stretching of tendons, muscles, and the components of joints. For example, have you ever stretched your muscles before or after exercise and noticed that you can only stretch so far before your muscles spasm back to a less stretched state? This spasm is a reflex that is initiated by stretch receptors to avoid muscle tearing. Such stretch receptors can also prevent over-contraction of a muscle. In skeletal muscle tissue, these stretch receptors are called muscle spindles. Golgi tendon organs similarly transduce the stretch levels of tendons. Bulbous corpuscles are also present in joint capsules, where they measure stretch in the components of the skeletal system within the joint. The types of nerve endings, their locations, and the stimuli they transduce are presented in Table 1.
| Table 1. Mechanoreceptors of Somatosensation | |||
|---|---|---|---|
| Name | Historical (eponymous) name | Location(s) | Stimuli |
| Free nerve endings | [No corresponding eponymous name] | Dermis, cornea, tongue, joint capsules, visceral organs | Pain, temperature, mechanical deformation |
| Mechanoreceptors | Merkel’s discs | Epidermal-dermal junction, mucosal membranes | Low frequency vibration (5-15 Hz) |
| Bulbous corpuscle | Ruffini’s corpuscle | Dermis, joint capsules | Stretch |
| Tactile corpuscle | Messiner’s corpuscle | Papillary dermis, especially in the fingertips and lips | Light touch, vibrations below 50 Hz |
| Lamellated corpuscle | Pacinian corpuscle | Deep dermis, subcutaneous tissue | Deep pressure, high-frequency vibration (around 250 Hz) |
| Hair folicle plexus | [No corresponding eponymous name] | Wrapped around hair follicles in the dermis | Movement of hair |
| Muscle spindle | [No corresponding eponymous name] | In line with skeletal muscle fibers | Muscle contraction and stretch |
| Tendon stretch organ | Golgi tendon organ | In line with tendons | Stretch of tendons |
Pain and Nociceptors
We have all felt pain, and although uncomfortable, it likely provided us important information about tissue damage — damage that may have gotten worse if pain had not made us aware of the problems at hand. In response to pain we tend to “protect” the damaged tissue from further use and seek appropriate medical attention. Thus pain is a critical sensation for alerting us to problems within the body such that they can be appropriately addressed.
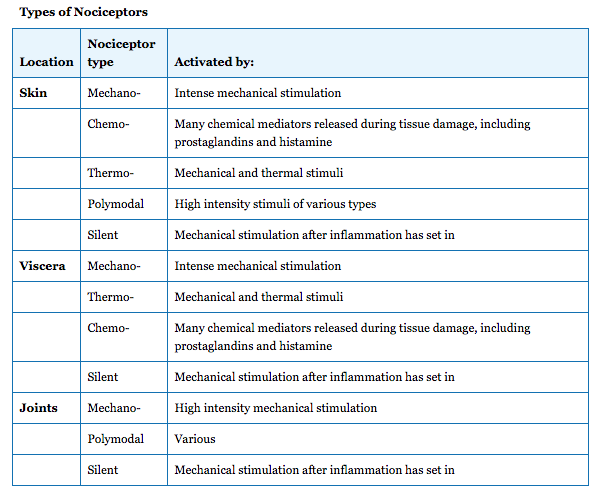
Pain receptors, called nociceptors, are spread throughout most of the body’s tissues, with the exception of the central nervous system. They respond to nociceptive, or noxious, stimuli that lead to our perception of pain. These receptors vary in the specific stimuli that they respond to, as well as how quickly they transmit information to the central nervous system.
You likely realize that there are many noxious stimuli. Extreme temperature, a pinch, blunt impact, cuts, intestinal gas, overuse of joints, and others can all elicit the sensation of pain. This is because all of these stimuli have the ability to either directly activate nociceptors, or cause tissue damage that leads to the release of chemical substances that will activate nociceptors. You also appreciate that the sensation of pain can change over time, where an injury may start out with stinging pain, become dull, and even revert to stinging again under certain conditions, such as when someone touches the injured area. The combination of nociceptors stimulated helps determine the characteristics of the pain that is felt. Examples of nociceptor locations and types are listed in Table below.
The silent (sleep) nociceptors listed in the table have the unique property that they are normally unresponsive to stimulation until turned “on” by chemicals released during the inflammatory process. This is one reason why, after you have stubbed your toe, or pinched your finger, you may have thought to yourself “this is going to hurt”. You know that once the tissue inflames (swells up), throbbing pain is likely to set in as further nociceptors become activated.
Besides the noxious stimulus that activates a receptor, the type of axon (fiber) that the receptor neuron contains also contributes to how we perceive pain. In general, fibers can be divided into 2 categories, with the properties listed in table below.
Categories of Pain
Because there are multiple types of nociceptors that can transmit information at different rates, our pain sensation is not always the same. Scientists generally recognize three different pain categories (sensations or stimulus modalities), as described in table below.

Characteristics of Pain
Hyperalgesia and Analgesia
Notice that because chemical and silent nociceptors are activated after tissue injury has set in, our sensations of pain can change over time. An initial cut will activate mechano-nociceptors, sending the fast pain signals along A-delta fibers to the brain. After inflammation in the area has set in, the chemical and/or silent nociceptors may send information along C fibers, producing a different pain sensation. If these silent nociceptors become sensitized by the inflammatory mediators, then we might experience hyperalgesia, where tissue stretch to an injured area can be sensed as a more intense pain.
Our ability to provide analgesia (reduce or block pain) is usually directed at inhibiting the local formation of the mediators that activate chemical nociceptors (this is how aspirin and ibuprofen work), blocking the transmission of signals along peripheral pain fibers (local anesthetics), or interrupting the transmission of pain signals in the CNS (endogenous or exogenous opioids as well as general anesthesia). You may have had experience with a local anesthetic during dental work or when stitches were put in. They act by blocking the ability of nerve fibers to conduct action potentials. Local anesthetics block C fibers more easily, but in time the A-delta fibers are also blocked. This is why the dentist waits awhile after giving the local anesthetic before commencing the work that would otherwise cause pain – you want to make sure your A-delta fibers are fully blocked as well!
CNS Role in Pain
Although the focus of this section has been on the peripheral sensation and transmission of resulting action potentials, keep in mind that the processing of pain, such as pain sensation, localization and the physical and emotional responses to pain, are functions of the CNS.
Candela Citations
- Anatomy & Physiology. Authored by: OpenStax College. Provided by: Rice University. Located at: http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@9.1. Project: Anatomy & Physiology. License: CC BY: Attribution. License Terms: Download for free at http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@9.1
- Unit 14: Nervous System (Module 56). Authored by: Open Learning Initiative. Provided by: Carnegie Mellon University. Located at: https://oli.cmu.edu/jcourse/workbook/activity/page?context=4348999280020ca600212ee04a7f1795. Project: Anatomy & Physiology. License: CC BY-NC-SA: Attribution-NonCommercial-ShareAlike
- Tactile Receptors.. Authored by: BruceBlaus. Provided by: Blausen.com staff (2014). Medical gallery of Blausen Medical 2014. Located at: https://commons.wikimedia.org/wiki/File:Blausen_0809_Skin_TactileReceptors.png. License: CC BY: Attribution