Nephrons: The Functional Units of the Kidney.
Nephrons take a simple filtrate of the blood and modify it into urine. Nephrons are the “functional units” of the kidney; they cleanse the blood and balance the constituents of the circulation. Each kidney is made up of over one million nephrons that dot the renal cortex, giving it a granular appearance when sectioned sagittally. Many changes take place in the different parts of the nephron before urine is created for disposal. The term forming urine will be used hereafter to describe the filtrate as it is modified into true urine. The principle task of the nephron population is to balance the plasma to homeostatic set points and excrete potential toxins in the urine. They do this by accomplishing three principle functions—filtration, reabsorption, and secretion. They also have additional secondary functions that exert control in three areas: blood pressure (via production of renin), red blood cell production (via the hormone EPO), and calcium absorption (via conversion of calcidiol into calcitriol, the active form of vitamin D).

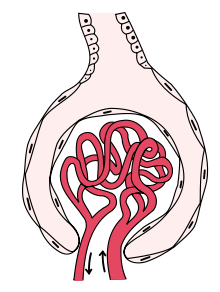
Figure 1. The nephron is the functional unit of the kidney. The glomerulus and convoluted tubules are located in the kidney cortex, while collecting ducts are located in the pyramids of the medulla. (credit: modification of work by NIDDK)
Tubular parts of a Nephron – converts the filtrate into urine
-
The Bowman’s capsule / Glomerular capsule:
The Bowman’s capsule (also called the glomerular capsule), is the beginning of a nephron. It surrounds the glomerulus. It is a double walled cup, It is composed of inner visceral and outer parietal layers. Parietal (outer) layer of glomerular capsule is simple squamous epithelium. Visceral (inner) layer of glomerular capsule consists of elaborate cells called podocytes that wrap around the capillaries of the glomerulus. Capsular space separates the two layers of glomerular capsule.
Renal tubule: long, coiled tube that converts the filtrate into urine
The renal tubule is a long and convoluted structure that emerges from the glomerular capsule and can be divided into three parts based on function. The first part is called the proximal convoluted tubule (PCT) due to its proximity to the glomerulus; it stays in the renal cortex. The second part is called the loop of Henle, because it forms a loop (with descending and ascending limbs) that goes through the renal medulla. The third part of the renal tubule is called the distal convoluted tubule (DCT) and this part is also restricted to the renal cortex. The DCT, which is the last part of the nephron, connects and empties its contents into collecting ducts that line the medullary pyramids. The collecting ducts amass contents from multiple nephrons and fuse together as they enter the papillae of the renal medulla.
- Proximal Convoluted Tubule: Filtered fluid collected by Bowman’s capsule enters into the PCT. It is called convoluted due to its tortuous path. Simple cuboidal cells form this tubule with prominent microvilli on the luminal surface, forming a brush border. These microvilli create a large surface area to maximize the absorption and secretion of solutes (Na+, Cl–, glucose, etc.), the most essential function of this portion of the nephron. These cells actively transport ions across their membranes, so they possess a high concentration of mitochondria in order to produce sufficient ATP.
- The loop of Henle is a U-shaped tube that consists of a descending limb and ascending limb. It transfers fluid from the proximal to the distal tubule. The descending and ascending portions of the loop of Henle (sometimes referred to as the nephron loop) are continuations of the same tubule. They run adjacent and parallel to each other after having made a hairpin turn at the deepest point of their descent. The descending loop of Henle consists of an initial short, thick portion and long, thin portion, whereas the ascending loop consists of an initial short, thin portion followed by a long, thick portion. The descending limb is highly permeable to water but completely impermeable to ions, causing a large amount of water to be reabsorbed, which increases fluid osmolarity to about 1200 mOSm/L. In contrast, the ascending limb of Henle’s loop is impermeable to water but highly permeable to ions, which causes a large drop in the osmolarity of fluid passing through the loop, from 1200 mOSM/L to 100 mOSm/L.

Figure 4. Tubular parts of Nephron and their functions.
-
Figure 5. Aquaporin Water Channel : Positive charges inside the channel prevent the leakage of electrolytes across the cell membrane, while allowing water to move due to osmosis.
- Distal Convoluted Tubule (DCT): The distal convoluted tubule and collecting duct is the final site of reabsorption in the nephron. Unlike the other components of the nephron, its permeability to water is variable depending on a hormone stimulus to enable the complex regulation of blood osmolarity, volume, pressure, and pH. The DCT, like the PCT, is very tortuous and formed by simple cuboidal epithelium, but it is shorter than the PCT. These cells are not as active as those in the PCT; thus, there are fewer microvilli on the apical surface. However, these cells must also pump ions against their concentration gradient, so you will find of large numbers of mitochondria, although fewer than in the PCT.
- Collecting Ducts: The collecting ducts are continuous with the nephron but not technically part of it. In fact, each duct collects filtrate from several nephrons for final modification. Collecting ducts merge as they descend deeper in the medulla to form about 30 terminal ducts, which empty at a papilla. They are lined with simple squamous epithelium with receptors for ADH. When stimulated by ADH, these cells will insert aquaporin channel proteins into their membranes, which as their name suggests, allow water to pass from the duct lumen through the cells and into the interstitial spaces to be recovered by the vasa recta. This process allows for the recovery of large amounts of water from the filtrate back into the blood. In the absence of ADH, these channels are not inserted, resulting in the excretion of water in the form of dilute urine. Most, if not all, cells of the body contain aquaporin molecules, whose channels are so small that only water can pass. At least 10 types of aquaporins are known in humans, and six of those are found in the kidney. The function of all aquaporins is to allow the movement of water across the lipid-rich, hydrophobic cell membrane.
Nephrons and Blood Vessels
Each nephron has its own independent blood supply.
- Afferent Arteriole: The renal artery first divides into smaller arteries, followed by further branching and pass through the renal columns to reach the cortex. In the cortex they divide further and form afferent arterioles.The afferent arterioles service about 1.3 million nephrons in each kidney. The branch that enters the glomerulus is called the afferent arteriole. A group of specialized cells known as juxtaglomerular apparatus (JGA) are located around the afferent arteriole where it enters the renal corpuscle. The JGA secretes an enzyme called renin, due to a variety of stimuli, and it is involved in the process of blood volume homeostasis.
-
The Glomerulus: The glomerulus is a capillary tuft that receives its blood supply from an afferent arteriole of the renal circulation. First step of urine formation “filtration of blood” happens at the glomerulular capillaries. – glomerular filtration. The glomerular capillaries are fenestrated capillaries. Fenestrated capillaries have pores in the endothelial cells those provide channels across the capillary wall so we could have small molecules pass through easily. These capillaries are more permeable than continuous capillaries. Fenestrations allow many substances to diffuse from the blood based primarily on size. Substances cross readily if they are less than 4 nm in size and most pass freely up to 8 nm in size. Water and small molecules like glucose, urea and ions like sodium cross the glomerular capillaries and get into the glomerular capsule of nephron. The fenestrations (pores) prevent filtration of blood cells or large proteins. Red blood cells and large proteins, such as serum albumins, cannot pass through the glomerulus under normal circumstances because they are too big to pass through glomerular capillaries. However, in some injuries they may be able to pass through and can cause blood and protein content to enter the urine, which is a sign of problems in the kidney. As blood passes through the glomerular capillaries, 10 to 20 percent of the plasma filters between these sieve-like fingers to be captured by Bowman’s capsule and funneled to the PCT. The glomerulus and the double walled cup-shaped chamber that surrounds it, called the glomerular or Bowman’s capsule, together is referred to as Renal corpuscle.

Figure 6: Fenestrated Capillary with fenestrations (pores) : Pores allow many substances to diffuse from the blood based primarily on size.
- Efferent Arteriole: After passing through the renal corpuscle, the capillaries form a second arteriole, the efferent arteriole The branch that exits the glomerulus is called the efferent arteriole. These will next form a capillary network around the more distal portions of the nephron tubule, the peritubular capillaries and vasa recta, before returning to the venous system. As the glomerular filtrate progresses through the nephron, these capillary networks recover most of the solutes and water, and return them to the circulation. Since a capillary bed (the glomerulus) drains into a vessel that in turn forms a second capillary bed, the definition of a portal system is met. This is the only portal system in which an arteriole is found between the first and second capillary beds.
- Peritubular capillaries: Peritubular capillaries are tiny blood vessels, supplied by the efferent arteriole, that travel alongside nephrons and surrounds them allowing reabsorption and secretion between blood and the inner lumen of the nephron. In cortical nephrons, the peritubular capillary network surrounds the PCT and DCT. In juxtamedullary nephrons, the peritubular capillary network forms a network around the loop of Henle and is called the vasa recta. Peritubular capillaries join together and form the renal veins and return the filtered blood with less waste materials to the venous system.
Candela Citations
- Anatomy & Physiology. Provided by: OpenStax CNX. Located at: http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.25. License: CC BY: Attribution. License Terms: Download for free at http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.25