Alcoholism is, broadly, any drinking of alcohol that results in significant mental or physical health problems.[14] Alcoholism is not a recognized diagnostic entity. Predominant diagnostic classifications are alcohol use disorder[2] (DSM-5)[4] or alcohol dependence (ICD-11).[15]
Signs and symptoms

The risk of alcohol dependence begins at low levels of drinking and increases directly with both the volume of alcohol consumed and a pattern of drinking larger amounts on an occasion, to the point of intoxication, which is sometimes called “binge drinking”.
Alcohol misuse
Some of the possible long-term effects of ethanol an individual may develop. Additionally, in pregnant women, alcohol can cause fetal alcohol syndrome.
Alcoholism is characterised by an increased tolerance to alcohol – which means that an individual can consume more alcohol – and physical dependence on alcohol, which makes it hard for an individual to control their consumption. The physical dependency caused by alcohol can lead to an affected individual having a very strong urge to drink alcohol. These characteristics play a role in decreasing an alcoholic’s ability to stop drinking.[29] Alcoholism can have adverse effects on mental health, contributing to psychiatric disorders and increasing the risk of suicide. A depressed mood is a common symptom of heavy alcohol drinkers.[30][31]
watch
Warning signs
Warning signs of alcoholism include the consumption of increasing amounts of alcohol and frequent intoxication, preoccupation with drinking to the exclusion of other activities, promises to quit drinking and failure to keep those promises, the inability to remember what was said or done while drinking (colloquially known as “blackouts”), personality changes associated with drinking, denial or the making of excuses for drinking, the refusal to admit excessive drinking, dysfunction or other problems at work or school, the loss of interest in personal appearance or hygiene, marital and economic problems, and the complaint of poor health, with loss of appetite, respiratory infections, or increased anxiety.[32]
Physical
Short-term effects
Drinking enough to cause a blood alcohol concentration (BAC) of 0.03–0.12% typically causes an overall improvement in mood and possible euphoria (a “happy” feeling), increased self-confidence and sociability, decreased anxiety, a flushed, red appearance in the face and impaired judgment and fine muscle coordination. A BAC of 0.09% to 0.25% causes lethargy, sedation, balance problems and blurred vision. A BAC of 0.18% to 0.30% causes profound confusion, impaired speech (e.g. slurred speech), staggering, dizziness and vomiting. A BAC from 0.25% to 0.40% causes stupor, unconsciousness, anterograde amnesia, vomiting (death may occur due to inhalation of vomit while unconscious) and respiratory depression (potentially life-threatening). A BAC from 0.35% to 0.80% causes a coma (unconsciousness), life-threatening respiratory depression and possibly fatal alcohol poisoning. With all alcoholic beverages, drinking while driving, operating an aircraft or heavy machinery increases the risk of an accident; many countries have penalties for drunk driving.
Long-term effects
Having more than one drink a day for women or two drinks for men increases the risk of heart disease, high blood pressure, atrial fibrillation, and stroke.[33] Risk is greater with binge drinking, which may also result in violence or accidents. About 3.3 million deaths (5.9% of all deaths) are believed to be due to alcohol each year.[13] Alcoholism reduces a person’s life expectancy by around ten years[26] and alcohol use is the third leading cause of early death in the United States.[33] No professional medical association recommends that people who are nondrinkers should start drinking.[33][34] Long-term alcohol misuse can cause a number of physical symptoms, including cirrhosis of the liver, pancreatitis, epilepsy, polyneuropathy, alcoholic dementia, heart disease, nutritional deficiencies, peptic ulcers[35] and sexual dysfunction, and can eventually be fatal. Other physical effects include an increased risk of developing cardiovascular disease, malabsorption, alcoholic liver disease, and several cancers. Damage to the central nervous system and peripheral nervous system can occur from sustained alcohol consumption.[36][37] A wide range of immunologic defects can result and there may be a generalized skeletal fragility, in addition to a recognized tendency to accidental injury, resulting a propensity to bone fractures.[38]
Women develop long-term complications of alcohol dependence more rapidly than do men. Additionally, women have a higher mortality rate from alcoholism than men.[39] Examples of long-term complications include brain, heart, and liver damage[40] and an increased risk of breast cancer. Additionally, heavy drinking over time has been found to have a negative effect on reproductive functioning in women. This results in reproductive dysfunction such as anovulation, decreased ovarian mass, problems or irregularity of the menstrual cycle, and early menopause.[39] Alcoholic ketoacidosis can occur in individuals who chronically misuse alcohol and have a recent history of binge drinking.[41][42] The amount of alcohol that can be biologically processed and its effects differ between sexes. Equal dosages of alcohol consumed by men and women generally result in women having higher blood alcohol concentrations (BACs), since women generally have a lower weight and higher percentage of body fat and therefore a lower volume of distribution for alcohol than men.[43]
Psychiatric
Long-term misuse of alcohol can cause a wide range of mental health problems. Severe cognitive problems are common; approximately 10 percent of all dementia cases are related to alcohol consumption, making it the second leading cause of dementia.[44] Excessive alcohol use causes damage to brain function, and psychological health can be increasingly affected over time.[45] Social skills are significantly impaired in people suffering from alcoholism due to the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain. The social skills that are impaired by alcohol use disorder include impairments in perceiving facial emotions, prosody, perception problems, and theory of mind deficits; the ability to understand humor is also impaired in people who misuse alcohol.[46] Psychiatric disorders are common in alcoholics, with as many as 25 percent suffering severe psychiatric disturbances. The most prevalent psychiatric symptoms are anxiety and depression disorders. Psychiatric symptoms usually initially worsen during alcohol withdrawal, but typically improve or disappear with continued abstinence.[47] Psychosis, confusion, and organic brain syndrome may be caused by alcohol misuse, which can lead to a misdiagnosis such as schizophrenia.[48] Panic disorder can develop or worsen as a direct result of long-term alcohol misuse.[49][50]
The co-occurrence of major depressive disorder and alcoholism is well documented.[51][52][53] Among those with comorbid occurrences, a distinction is commonly made between depressive episodes that remit with alcohol abstinence (“substance-induced”), and depressive episodes that are primary and do not remit with abstinence (“independent” episodes).[54][55][56] Additional use of other drugs may increase the risk of depression.[57] Psychiatric disorders differ depending on gender. Women who have alcohol-use disorders often have a co-occurring psychiatric diagnosis such as major depression, anxiety, panic disorder, bulimia, post-traumatic stress disorder (PTSD), or borderline personality disorder. Men with alcohol-use disorders more often have a co-occurring diagnosis of narcissistic or antisocial personality disorder, bipolar disorder, schizophrenia, impulse disorders or attention deficit/hyperactivity disorder (ADHD).[58] Women with alcohol use disorder are more likely to experience physical or sexual assault, abuse, and domestic violence than women in the general population,[58] which can lead to higher instances of psychiatric disorders and greater dependence on alcohol.
Social effects
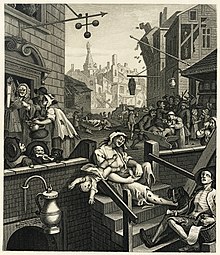
Serious social problems arise from alcohol use disorder; these dilemmas are caused by the pathological changes in the brain and the intoxicating effects of alcohol.[44][59] Alcohol misuse is associated with an increased risk of committing criminal offences, including child abuse, domestic violence, rape, burglary and assault.[60] Alcoholism is associated with loss of employment,[61] which can lead to financial problems. Drinking at inappropriate times and behavior caused by reduced judgment can lead to legal consequences, such as criminal charges for drunk driving[62] or public disorder, or civil penalties for tortious behavior. An alcoholic’s behavior and mental impairment while drunk can profoundly affect those surrounding him and lead to isolation from family and friends. This isolation can lead to marital conflict and divorce, or contribute to domestic violence. Alcoholism can also lead to child neglect, with subsequent lasting damage to the emotional development of the alcoholic’s children.[63] For this reason, children of alcoholic parents can develop a number of emotional problems. For example, they can become afraid of their parents, because of their unstable mood behaviors. In addition, they can develop considerable amount of shame over their inadequacy to liberate their parents from alcoholism. As a result of this failure, they develop wretched self-images, which can lead to depression.[64]
Alcohol withdrawal
Severe acute withdrawal symptoms such as delirium tremens and seizures rarely occur after 1-week post cessation of alcohol. The acute withdrawal phase can be defined as lasting between one and three weeks. In the period of 3–6 weeks following cessation, anxiety, depression, fatigue, and sleep disturbance are common.[69] Similar post-acute withdrawal symptoms have also been observed in animal models of alcohol dependence and withdrawal.[70]
A kindling effect also occurs in alcoholics whereby each subsequent withdrawal syndrome is more severe than the previous withdrawal episode; this is due to neuroadaptations which occur as a result of periods of abstinence followed by re-exposure to alcohol. Individuals who have had multiple withdrawal episodes are more likely to develop seizures and experience more severe anxiety during withdrawal from alcohol than alcohol-dependent individuals without a history of past alcohol withdrawal episodes. The kindling effect leads to persistent functional changes in brain neural circuits as well as to gene expression.[71] Kindling also results in the intensification of psychological symptoms of alcohol withdrawal.[69] There are decision tools and questionnaires that help guide physicians in evaluating alcohol withdrawal. For example, the CIWA-Ar objectifies alcohol withdrawal symptoms in order to guide therapy decisions which allows for an efficient interview while at the same time retaining clinical usefulness, validity, and reliability, ensuring proper care for withdrawal patients, who can be in danger of death.[72]
Causes
Severe childhood trauma is also associated with a general increase in the risk of drug dependency.[73] Lack of peer and family support is associated with an increased risk of alcoholism developing.[73] Genetics and adolescence are associated with an increased sensitivity to the neurotoxic effects of chronic alcohol use. Cortical degeneration due to the neurotoxic effects increases impulsive behaviour, which may contribute to the development, persistence and severity of alcohol use disorders. There is evidence that with abstinence, there is a reversal of at least some of the alcohol induced central nervous system damage.[77] The use of cannabis was associated with later problems with alcohol use.[78] Alcohol use was associated with an increased probability of later use of tobacco and illegal drugs such as cannabis.[79]
Screening
Screening is recommended among those over the age of 18.[111] Several tools may be used to detect a loss of control of alcohol use. These tools are mostly self-reports in questionnaire form. Another common theme is a score or tally that sums up the general severity of alcohol use.[112]
The CAGE questionnaire, named for its four questions, is one such example that may be used to screen patients quickly in a doctor’s office.
Two “yes” responses indicate that the respondent should be investigated further.
The questionnaire asks the following questions:
- Have you ever felt you needed to Cut down on your drinking?
- Have people Annoyed you by criticizing your drinking?
- Have you ever felt Guilty about drinking?
- Have you ever felt you needed a drink first thing in the morning (Eye-opener) to steady your nerves or to get rid of a hangover?
- The CAGE questionnaire has demonstrated a high effectiveness in detecting alcohol-related problems; however, it has limitations in people with less severe alcohol-related problems, white women and college students.
Other tests are sometimes used for the detection of alcohol dependence, such as the Alcohol Dependence Data Questionnaire, which is a more sensitive diagnostic test than the CAGE questionnaire. It helps distinguish a diagnosis of alcohol dependence from one of heavy alcohol use.[116] The Michigan Alcohol Screening Test (MAST) is a screening tool for alcoholism widely used by courts to determine the appropriate sentencing for people convicted of alcohol-related offenses,[117] driving under the influence being the most common. The Alcohol Use Disorders Identification Test (AUDIT), a screening questionnaire developed by the World Health Organization, is unique in that it has been validated in six countries and is used internationally. Like the CAGE questionnaire, it uses a simple set of questions – a high score earning a deeper investigation.[118] The Paddington Alcohol Test (PAT) was designed to screen for alcohol-related problems amongst those attending Accident and Emergency departments. It concords well with the AUDIT questionnaire but is administered in a fifth of the time.[119]
Management
Treatments are varied because there are multiple perspectives of alcoholism. Those who approach alcoholism as a medical condition or disease recommend differing treatments from, for instance, those who approach the condition as one of social choice. Most treatments focus on helping people discontinue their alcohol intake, followed up with life training and/or social support to help them resist a return to alcohol use. Since alcoholism involves multiple factors which encourage a person to continue drinking, they must all be addressed to successfully prevent a relapse. An example of this kind of treatment is detoxification followed by a combination of supportive therapy, attendance at self-help groups, and ongoing development of coping mechanisms. Much of the treatment community for alcoholism supports an abstinence-based zero tolerance approach; however, some prefer a harm-reduction approach.[125]
Detoxification
Alcohol detoxification or ‘detox’ for alcoholics is an abrupt stop of alcohol drinking coupled with the substitution of drugs, such as benzodiazepines, that have similar effects to prevent alcohol withdrawal. Individuals who are only at risk of mild to moderate withdrawal symptoms can be detoxified as outpatients. Individuals at risk of a severe withdrawal syndrome as well as those who have significant or acute comorbid conditions are generally treated as inpatients. Detoxification does not actually treat alcoholism, and it is necessary to follow up detoxification with an appropriate treatment program for alcohol dependence or alcohol use disorder to reduce the risk of relapse.[9] Some symptoms of alcohol withdrawal such as depressed mood and anxiety typically take weeks or months to abate while other symptoms persist longer due to persisting neuroadaptations.[69] Alcoholism has serious adverse effects on brain function; on average it takes one year of abstinence to recover from the cognitive deficits incurred by chronic alcohol misuse.[126]
Psychological
Moderate drinking
Rationing and moderation programs such as Moderation Management and DrinkWise do not mandate complete abstinence. While most alcoholics are unable to limit their drinking in this way, some return to moderate drinking. A 2002 US study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) showed that 17.7 percent of individuals diagnosed as alcohol dependent more than one year prior returned to low-risk drinking. This group, however, showed fewer initial symptoms of dependency.[129]
A follow-up study, using the same subjects that were judged to be in remission in 2001–2002, examined the rates of return to problem drinking in 2004–2005. The study found abstinence from alcohol was the most stable form of remission for recovering alcoholics.[130] There was also a 1973 study showing chronic alcoholics drinking moderately again,[131] but a 1982 follow-up showed that 95% of subjects were not able to moderately drink over the long term.[132][133] Another study was a long-term (60 year) follow-up of two groups of alcoholic men which concluded that “return to controlled drinking rarely persisted for much more than a decade without relapse or evolution into abstinence.”[134] Internet based measures appear to be useful at least in the short term.[135]
Medications
Disulfiram-like drug
In the United States there are four approved medications for alcoholism: acamprosate, two methods of using naltrexone and disulfiram.[136]
- Acamprosate may stabilise the brain chemistry that is altered due to alcohol dependence via antagonising the actions of glutamate, a neurotransmitter which is hyperactive in the post-withdrawal phase.[137] By reducing excessive NMDA activity which occurs at the onset of alcohol withdrawal, acamprosate can reduce or prevent alcohol withdrawal related neurotoxicity.[138] Acamprosate reduces the risk of relapse amongst alcohol-dependent persons.[139][140]
- Naltrexone is a competitive antagonist for opioid receptors, effectively blocking the effects of endorphins and opioids. Naltrexone is used to decrease cravings for alcohol and encourage abstinence. Alcohol causes the body to release endorphins, which in turn release dopamine and activate the reward pathways; hence in the body reduces the pleasurable effects from consuming alcohol.[141] Evidence supports a reduced risk of relapse among alcohol-dependent persons and a decrease in excessive drinking.[140] Nalmefene also appears effective and works in a similar manner.[140]
- The Sinclair method is another approach to using naltrexone or other opioid antagonists to treat alcoholism by having the person take the medication about an hour before they drink alcohol and only then.[142][143] The medication blocks the positive reinforcement effects of ethanol and hypothetically allows the person to stop drinking or drink less.[143]
- Disulfiram prevents the elimination of acetaldehyde, a chemical the body produces when breaking down ethanol. Acetaldehyde itself is the cause of many hangover symptoms from alcohol use. The overall effect is discomfort when alcohol is ingested: an extremely fast-acting and long-lasting, uncomfortable hangover.
Several other drugs are also used and many are under investigation.
- Benzodiazepines, while useful in the management of acute alcohol withdrawal, if used long-term can cause a worse outcome in alcoholism. Alcoholics on chronic benzodiazepines have a lower rate of achieving abstinence from alcohol than those not taking benzodiazepines. This class of drugs is commonly prescribed to alcoholics for insomnia or anxiety management.[144] Initiating prescriptions of benzodiazepines or sedative-hypnotics in individuals in recovery has a high rate of relapse with one author reporting more than a quarter of people relapsed after being prescribed sedative-hypnotics. Those who are long-term users of benzodiazepines should not be withdrawn rapidly, as severe anxiety and panic may develop, which are known risk factors for alcohol use disorder relapse. Taper regimes of 6–12 months have been found to be the most successful, with reduced intensity of withdrawal.[145][146]
- Calcium carbimide works in the same way as disulfiram; it has an advantage in that the occasional adverse effects of disulfiram, hepatotoxicity and drowsiness, do not occur with calcium carbimide.[147]
- Ondansetron and topiramate are supported by tentative evidence in people with certain genetics.[148][149] Evidence for ondansetron is more in those who have just begun having problems with alcohol.[148] Topiramate is a derivative of the naturally occurring sugar monosaccharide D-fructose. Review articles characterize topiramate as showing “encouraging”,[148] “promising”,[148] “efficacious”,[150] and “insufficient”[151] evidence in the treatment of alcohol use disorders.
Evidence does not support the use of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), antipsychotics, or gabapentin.[140]
Dual addictions and dependences
Alcoholics may also require treatment for other psychotropic drug addictions and drug dependences. The most common dual dependence syndrome with alcohol dependence is benzodiazepine dependence, with studies showing 10–20 percent of alcohol-dependent individuals had problems of dependence and/or misuse problems of benzodiazepine drugs such as diazepam or clonazepam. These drugs are, like alcohol, depressants. Benzodiazepines may be used legally, if they are prescribed by doctors for anxiety problems or other mood disorders, or they may be purchased as illegal drugs. Benzodiazepine use increases cravings for alcohol and the volume of alcohol consumed by problem drinkers.[152] Benzodiazepine dependency requires careful reduction in dosage to avoid benzodiazepine withdrawal syndrome and other health consequences. Dependence on other sedative-hypnotics such as zolpidem and zopiclone as well as opiates and illegal drugs is common in alcoholics. Alcohol itself is a sedative-hypnotic and is cross-tolerant with other sedative-hypnotics such as barbiturates, benzodiazepines and nonbenzodiazepines. Dependence upon and withdrawal from sedative-hypnotics can be medically severe and, as with alcohol withdrawal, there is a risk of psychosis or seizures if not properly managed.[153]
Candela Citations
- Alcoholism. Provided by: Wikimedia, inc. Located at: https://en.wikipedia.org/wiki/Alcoholism. License: CC BY-SA: Attribution-ShareAlike