Classification
There are several diseases where joint pain is primary, and is considered the main feature. Generally when a person has “arthritis” it means that they have one of these diseases, which include:
- Osteoarthritis
- Rheumatoid arthritis
- Gout and pseudo-gout
- Septic arthritis
- Ankylosing spondylitis
- Juvenile idiopathic arthritis
- Still’s disease
Joint pain can also be a symptom of other diseases. In this case, the arthritis is considered to be secondary to the main disease; these include:
- Psoriasis (Psoriatic arthritis)
- Reactive arthritis
- Ehlers–Danlos syndrome
- Haemochromatosis
- Hepatitis
- Lyme disease
- Sjögren’s disease
- Hashimoto’s thyroiditis
- Celiac disease[15]
- Non-celiac gluten sensitivity[16][17][18]
- Inflammatory bowel disease (including Crohn’s disease and ulcerative colitis)
- Henoch–Schönlein purpura
- Hyperimmunoglobulinemia D with recurrent fever
- Sarcoidosis
- Whipple’s disease
- TNF receptor associated periodic syndrome
- Granulomatosis with polyangiitis (and many other vasculitis syndromes)
- Familial Mediterranean fever
- Systemic lupus erythematosus
An undifferentiated arthritis is an arthritis that does not fit into well-known clinical disease categories, possibly being an early stage of a definite rheumatic disease.[19]
Signs and symptoms
| Extra-articular features of joint disease[20] |
|---|
| Cutaneous nodules |
| Cutaneous vasculitis lesions |
| Lymphadenopathy |
| Oedema |
| Ocular inflammation |
| Urethritis |
| Tenosynovitis (tendon sheath effusions) |
| Bursitis (swollen bursa) |
| Diarrhea |
| Orogenital ulceration |
Pain, which can vary in severity, is a common symptom in virtually all types of arthritis. Other symptoms include swelling, joint stiffness, redness, and aching around the joint(s).[2] Arthritic disorders like lupus and rheumatoid arthritis can affect other organs in the body, leading to a variety of symptoms.[21] Symptoms may include:[2]
- Inability to use the hand or walk
- Stiffness in one or more joints
- Rash or itch
- Malaise and fatigue
- Weight loss
- Poor sleep
- Muscle aches and pains
- Tenderness
- Difficulty moving the joint
It is common in advanced arthritis for significant secondary changes to occur. For example, arthritic symptoms might make it difficult for a person to move around and/or exercise, which can lead to secondary effects, such as:
Disability
Arthritis is the most common cause of disability in the United States. More than 20 million individuals with arthritis have severe limitations in function on a daily basis.[22] Absenteeism and frequent visits to the physician are common in individuals who have arthritis. Arthritis can make it very difficult for individuals to be physically active and some become home bound.
It is estimated that the total cost of arthritis cases is close to $100 billion of which almost 50% is from lost earnings. Each year, arthritis results in nearly 1 million hospitalizations and close to 45 million outpatient visits to health care centers.[23]
Decreased mobility, in combination with the above symptoms, can make it difficult for an individual to remain physically active, contributing to an increased risk of obesity, high cholesterol or vulnerability to heart disease.[24] People with arthritis are also at increased risk of depression, which may be a response to numerous factors, including fear of worsening symptoms.[25]
Risk factors
There are common risk factors that increase a person’s chance of developing arthritis later in adulthood. Some of these are modifiable while others are not. [26] Smoking has been linked to an increased susceptibility of developing arthritis, particularly rheumatoid arthritis.[27]
Diagnosis
Diagnosis is made by clinical examination from an appropriate health professional, and may be supported by other tests such as radiology and blood tests, depending on the type of suspected arthritis.[28] All arthritides potentially feature pain. Pain patterns may differ depending on the arthritides and the location. Rheumatoid arthritis is generally worse in the morning and associated with stiffness lasting over 30 minutes.[29] However, in the early stages, patients may have no symptoms after a warm shower. Osteoarthritis, on the other hand, tends to be associated with morning stiffness which eases relatively quickly with movement and exercise. In the aged and children, pain might not be the main presenting feature; the aged patient simply moves less, the infantile patient refuses to use the affected limb.
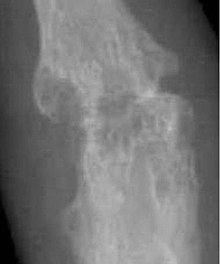
Elements of the history of the disorder guide diagnosis. Important features are speed and time of onset, pattern of joint involvement, symmetry of symptoms, early morning stiffness, tenderness, gelling or locking with inactivity, aggravating and relieving factors, and other systemic symptoms. Physical examination may confirm the diagnosis, or may indicate systemic disease. Radiographs are often used to follow progression or help assess severity.
Blood tests and X-rays of the affected joints often are performed to make the diagnosis. Screening blood tests are indicated if certain arthritides are suspected. These might include: rheumatoid factor, antinuclear factor (ANF), extractable nuclear antigen, and specific antibodies.
Osteoarthritis
Osteoarthritis is the most common form of arthritis.[30] It affects humans and other animals, notably dogs, but also occurs in cats and horses. It can affect both the larger and the smaller joints of the body. In humans, this included the hands, wrists, feet, back, hip, and knee. In dogs, this includes the elbow, hip, stifle (knee), shoulder, and back. The disease is essentially one acquired from daily wear and tear of the joint; however, osteoarthritis can also occur as a result of injury. Osteoarthritis begins in the cartilage and eventually causes the two opposing bones to erode into each other. The condition starts with minor pain during physical activity, but soon the pain can be continuous and even occur while in a state of rest. The pain can be debilitating and prevent one from doing some activities. In dogs, this pain can significantly affect quality of life and may include difficulty going up and down stairs, struggling to get up after lying down, trouble walking on slick floors, being unable to hop in and out of vehicles, difficulty jumping on and off furniture, and behavioral changes (e.g., aggression, difficulty squatting to toilet).[31] Osteoarthritis typically affects the weight-bearing joints, such as the back, knee and hip. Unlike rheumatoid arthritis, osteoarthritis is most commonly a disease of the elderly. The strongest predictor of osteoarthritis is increased age, likely due to the declining ability of chondrocytes to maintain the structural integrity of cartilage.[32] More than 30 percent of women have some degree of osteoarthritis by age 65. Other risk factors for osteoarthritis include prior joint trauma, obesity, and a sedentary lifestyle.[33]
Rheumatoid arthritis
Bone erosion is a central feature of rheumatoid arthritis. Bone continuously undergoes remodeling by actions of bone resorbing osteoclasts and bone forming osteoblasts. One of the main triggers of bone erosion in the joints in rheumatoid arthritis is inflammation of the synovium, caused in part by the production of pro-inflammatory cytokines and receptor activator of nuclear factor kappa B ligand (RANKL), a cell surface protein present in Th17 cells and osteoblasts.[40] Osteoclast activity can be directly induced by osteoblasts through the RANK/RANKL mechanism.[41]
Lupus
Lupus is a common collagen vascular disorder that can be present with severe arthritis. Other features of lupus include a skin rash, extreme photosensitivity, hair loss, kidney problems, lung fibrosis and constant joint pain.[42]
Gout
Gout is caused by deposition of uric acid crystals in the joint, causing inflammation. There is also an uncommon form of gouty arthritis caused by the formation of rhomboid crystals of calcium pyrophosphate known as pseudogout. In the early stages, the gouty arthritis usually occurs in one joint, but with time, it can occur in many joints and be quite crippling. The joints in gout can often become swollen and lose function. Gouty arthritis can become particularly painful and potentially debilitating when gout cannot successfully be treated.[43] When uric acid levels and gout symptoms cannot be controlled with standard gout medicines that decrease the production of uric acid (e.g., allopurinol) or increase uric acid elimination from the body through the kidneys (e.g., probenecid), this can be referred to as refractory chronic gout.[44]
Comparison of types
| Osteoarthritis | Rheumatoid arthritis | Gouty arthritis | |
|---|---|---|---|
| Speed of onset | Months | Weeks-months[46] | Hours for an attack[47] |
| Main locations | Weight-bearing joints (such as knees, hips, vertebral column) and hands | Hands (proximal interphalangeal and metacarpophalangeal joint) wrists, ankles, knees and hips | Great toe, ankles, knees and elbows |
| Inflammation | May occur, though often mild compared to inflammation in rheumatoid arthritis | Yes | Yes |
| Radiologic changes |
|
|
|
| Laboratory findings | None | Anemia, elevated ESR and C-reactive protein (CRP), rheumatoid factor, anti-citrullinated protein antibody | Crystal in joints |
| Other features |
|
|
Other
Infectious arthritis is another severe form of arthritis. It presents with sudden onset of chills, fever and joint pain. The condition is caused by bacteria elsewhere in the body. Infectious arthritis must be rapidly diagnosed and treated promptly to prevent irreversible joint damage.[48]
Psoriasis can develop into psoriatic arthritis. With psoriatic arthritis, most individuals develop the skin problem first and then the arthritis. The typical features are of continuous joint pains, stiffness and swelling. The disease does recur with periods of remission but there is no cure for the disorder. A small percentage develop a severe painful and destructive form of arthritis which destroys the small joints in the hands and can lead to permanent disability and loss of hand function.[49]
Treatment
There is no known cure for arthritis and rheumatic diseases. Treatment options vary depending on the type of arthritis and include physical therapy, exercise and diet, orthopedic bracing, and oral and topical medications.[2][50] Joint replacement surgery may be required to repair damage, restore function, or relieve pain.[2]
Physical therapy
In general, studies have shown that physical exercise of the affected joint can noticeably improve long-term pain relief. Furthermore, exercise of the arthritic joint is encouraged to maintain the health of the particular joint and the overall body of the person.[51]
Individuals with arthritis can benefit from both physical and occupational therapy. In arthritis the joints become stiff and the range of movement can be limited. Physical therapy has been shown to significantly improve function, decrease pain, and delay need for surgical intervention in advanced cases.[52] Exercise prescribed by a physical therapist has been shown to be more effective than medications in treating osteoarthritis of the knee. Exercise often focuses on improving muscle strength, endurance and flexibility. In some cases, exercises may be designed to train balance. Occupational therapy can provide assistance with activities. Assistive technology is a tool used to aid a person’s disability by reducing their physical barriers by improving the use of their damaged body part, typically after an amputation. Assistive technology devices can be customized to the patient or bought commercially.[53]
Medications
There are several types of medications that are used for the treatment of arthritis. Treatment typically begins with medications that have the fewest side effects with further medications being added if insufficiently effective.[54]
Depending on the type of arthritis, the medications that are given may be different. For example, the first-line treatment for osteoarthritis is acetaminophen (paracetamol) while for inflammatory arthritis it involves non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen. Opioids and NSAIDs may be less well tolerated.[55] However, topical NSAIDs may have better safety profiles than oral NSAIDs. For more severe cases of osteoarthritis, intra-articular corticosteroid injections may also be considered.[56]
The drugs to treat rheumatoid arthritis (RA) range from corticosteroids to monoclonal antibodies given intravenously. Due to the autoimmune nature of RA, treatments may include not only pain medications and anti-inflammatory drugs, but also another category of drugs called disease-modifying antirheumatic drugs (DMARDs). Treatment with DMARDs is designed to slow down the progression of RA by initiating an adaptive immune response, in part by CD4+ T helper (Th) cells, specifically Th17 cells.[57] Th17 cells are present in higher quantities at the site of bone destruction in joints and produce inflammatory cytokines associated with inflammation, such as interleukin-17 (IL-17).[40]
Surgery
A number of rheumasurgical interventions have been incorporated in the treatment of arthritis since the 1950s. Arthroscopic surgery for osteoarthritis of the knee provides no additional benefit to optimized physical and medical therapy.[58]
Adaptive aids
People with hand arthritis can have trouble with simple activities of daily living tasks (ADLs), such as turning a key in a lock or opening jars, as these activities can be cumbersome and painful. There are adaptive aids or (assistive devices (ADs)) available to help with these tasks,[59] but they are generally more costly than conventional products with the same function. It is now possible to 3-D print adaptive aids, which have been released as open source hardware to reduce patient costs.[60][61] Adaptive aids can significantly help arthritis patients and the vast majority of those with arthritis need and use them.[62]
Alternative medicine
Further research is required to determine if transcutaneous electrical nerve stimulation (TENS) for knee osteoarthritis is effective for controlling pain.[63]
Low level laser therapy may be considered for relief of pain and stiffness associated with arthritis.[64] Evidence of benefit is tentative.[65]
Pulsed electromagnetic field therapy (PEMFT) has tentative evidence supporting improved functioning but no evidence of improved pain in osteoarthritis.[66] The FDA has not approved PEMFT for the treatment of arthritis. In Canada, PEMF devices are legally licensed by Health Canada for the treatment of pain associated with arthritic conditions.[67]