Every player on a softball team has a special job to perform. Each of the orange team’s players in Figure 10.6.110.6.1 has his part of the infield or outfield covered if the ball comes his way. Other players on the orange team cover other parts of the field or pitch or catch the ball. Playing softball clearly requires teamwork. The human body is like a softball team in that regard. All the organ systems of the human body must work together as a team to keep the body alive and well. Teamwork within the body begins with communication.

Communication among Organ Systems
Communication among organ systems is vital if they are to work together as a team. They must be able to respond to each other and change their responses as needed to keep the body in balance. Communication among organ systems is controlled mainly by the autonomic nervous system and the endocrine system.
The autonomic nervous system is the part of the nervous system that controls involuntary functions. For example, the autonomic nervous system controls heart rate, blood flow, and digestion. You don’t have to tell your heart to beat faster or to consciously squeeze muscles to push food through the digestive system. In fact, you don’t have to even think about these functions at all. The autonomic nervous system orchestrates all the signals needed to control them. It sends messages between parts of the nervous system and between the nervous system and other organ systems via chemical messengers called neurotransmitters.

Figure 10.6.210.6.2: The figure illustrates the hypothalamus, pituitary gland, brain stem, spinal cord, cerebellum, pineal gland, and cerebrum. (Mandeep Grewal modified from Public domain; National Cancer Institute via Wikimedia.org)
The endocrine system is the system of glands that secrete hormones directly into the bloodstream. Once in the blood, endocrine hormones circulate to cells everywhere in the body. The endocrine system is under control of the hypothalamus, a part of the brain. The hypothalamus secretes hormones that travel directly to cells of the pituitary gland, which is located beneath it. The pituitary gland is the master gland of the endocrine system. Most of its hormones either turn on or turn off other endocrine glands. For example, if the pituitary gland secretes thyroid stimulating hormone, the hormone travels through the circulation to the thyroid gland, which is stimulated to secrete thyroid hormone. Thyroid hormone then travels to cells throughout the body, where it increases their metabolism.
Examples of Organ System Interactions
An increase in cellular metabolism requires more cellular respiration. Cellular respiration is a good example of organ system interactions because it is a basic life process that occurs in all living cells.
Cellular Respiration
Cellular respiration is the intracellular process that breaks down glucose with oxygen to produce carbon dioxide and energy in the form of ATP molecules. It is the process by which cells obtain usable energy to power other cellular processes. Which organ systems are involved in cellular respiration? The glucose needed for cellular respiration comes from the digestive system via the cardiovascular system. The oxygen needed for cellular respiration comes from the respiratory system also via the cardiovascular system. The carbon dioxide produced in cellular respiration leaves the body by the opposite route. In short, cellular respiration requires at a minimum the digestive, cardiovascular, and respiratory systems.
Fight-or-Flight Response
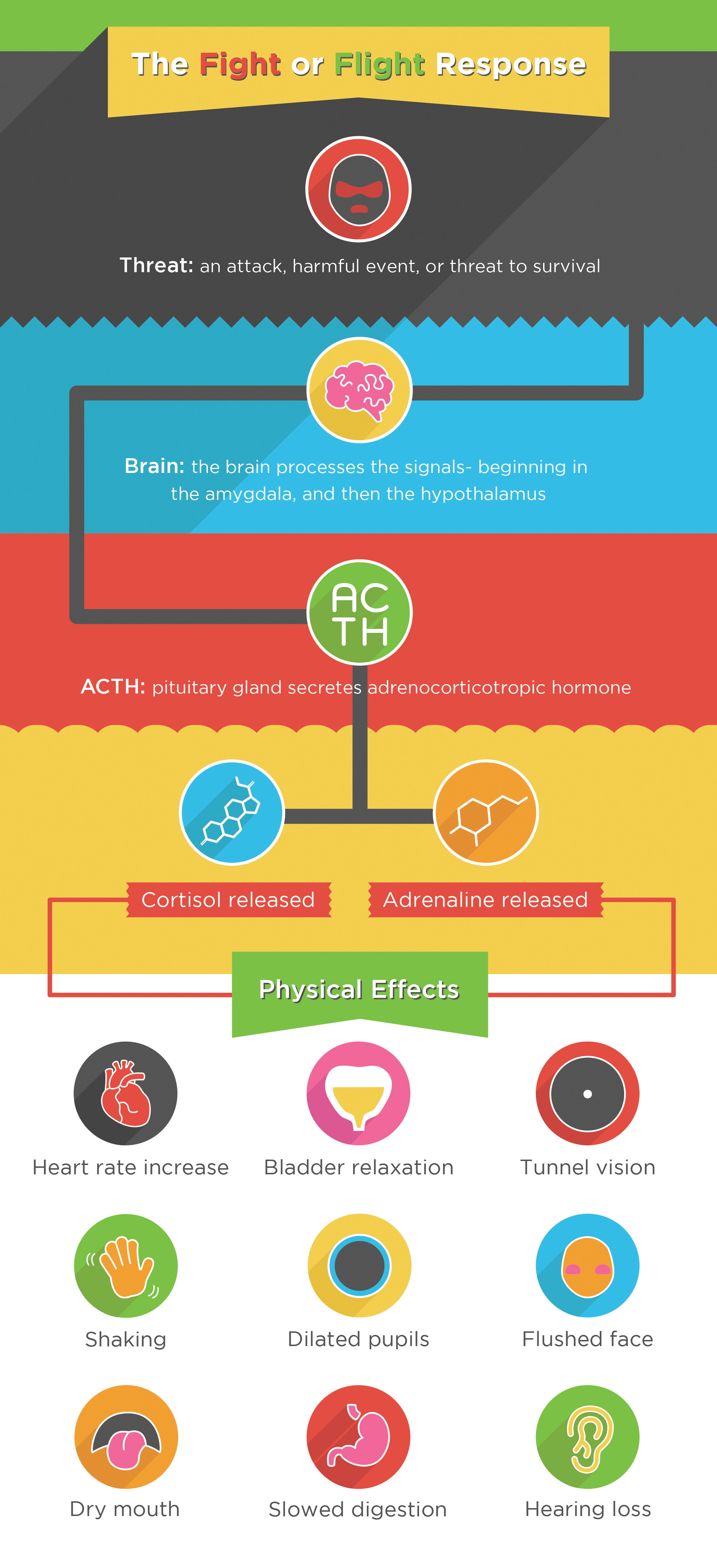
The well-known fight-or-flight response is a good example of how the nervous and endocrine systems control other organ system responses. The fight-or-flight response begins when the nervous system perceives sudden danger, as shown in Figure 10.6.210.6.2. The brain sends a message to the endocrine system (via the pituitary gland) for the adrenal glands to secrete their hormones cortisol and adrenaline. These hormones flood the circulation and affect other organ systems throughout the body, including the cardiovascular, urinary, sensory, and digestive systems. Specific responses include increased heart rate, bladder relaxation, tunnel vision, and a shunting of blood away from the digestive system and toward the muscles, brain, and other vital organs needed to fight or flee.
Digesting Food
Digesting food requires teamwork between the digestive system and several other organ systems, including the nervous, cardiovascular, and muscular systems. When you eat a meal, the organs of the digestive system need more blood to perform their digestive functions. Food entering the digestive systems causes nerve impulses to be sent to the brain; in response, the brain sends messages to the cardiovascular system to increase heart rate and dilate blood vessels in the digestive organs. Food passes through the organs of the digestive tract by rhythmic contractions of smooth muscles in the walls of the organs, so the muscular system is also needed for digestion. After food is digested, nutrients from the food are absorbed into the blood of the vessels lining the small intestine. Any remaining food waste is excreted through the large intestine.
Playing Softball
The men playing softball in Figure 10.6.110.6.1 are using multiple organ systems in this voluntary activity. Their nervous systems are focused on observing and preparing to respond to the next play. Their other systems are being controlled by the autonomic nervous system. Organ systems they are using include the muscular, skeletal, respiratory, and cardiovascular systems. Can you explain how each of these organ systems is involved in playing softball?
Exercises
Learn more about type 1 diabetes. Use several reliable Internet sources to answer the following questions:
- What causes the endocrine system to fail to produce insulin in type 1 diabetes?
- Which organ systems are affected by high blood glucose levels if type 1 diabetes is not controlled? What are some of the specific effects?
- How can blood glucose levels be controlled in patients with type 1 diabetes?
Homeostasis and Feedback
Steady as She Goes
This device looks simple, but it controls a complex system that keeps a home at a steady temperature. The device is an old-fashioned thermostat. The dial shows the current temperature in the room and also allows the occupant to set the thermostat to the desired temperature. A thermostat is a commonly cited model of how living systems, including the human body, maintain a steady state called homeostasis.

What is Homeostasis?
Homeostasis is the condition in which a system such as the human body is maintained in a more-or-less steady state. It is the job of cells, tissues, organs, and organ systems throughout the body to maintain many different variables within narrow ranges that are compatible with life. Keeping a stable internal environment requires continuous monitoring of the internal environment and constantly making adjustments to keep things in balance.
Set Point and Normal Range
For any given variable, such as body temperature or blood glucose level, there is a particular set point that is the physiological optimum value. For example, the set point for human body temperature is about 37 ºC (98.6 ºF). As the body works to maintain homeostasis for temperature or any other internal variable, the value typically fluctuates around the set point. Such fluctuations are normal as long as they do not become too extreme. The spread of values within which such fluctuations are considered insignificant is called the normal range. In the case of body temperature, for example, the normal range for an adult is about 36.5 to 37.5 ºC (97.7 to 99.5 ºF).
Maintaining Homeostasis
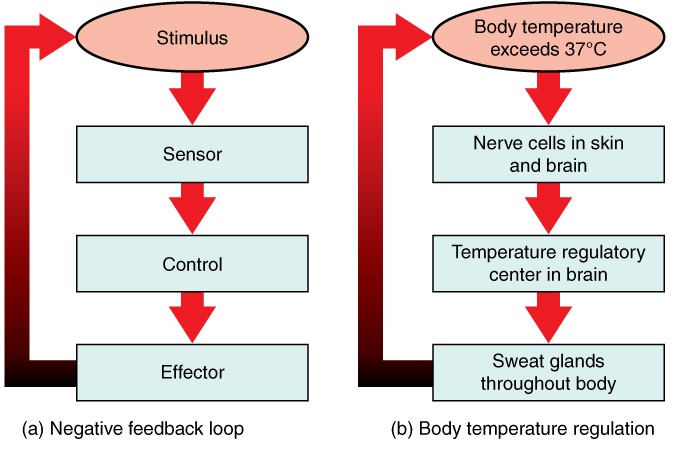
Homeostasis is normally maintained in the human body by an extremely complex balancing act. Regardless of the variable being kept within its normal range, maintaining homeostasis requires at least four interacting components: stimulus, sensor, control center, and effector.
- The stimulus is provided by the variable that is being regulated. Generally, the stimulus indicates that the value of the variable has moved away from the set point or has left the normal range.
- The sensor monitors the values of the variable and sends data on it to the control center.
- The control center matches the data with normal values. If the value is not at the set point or is outside the normal range, the control center sends a signal to the effector.
- The effector is an organ, gland, muscle, or other structure that acts on the signal from the control center to move the variable back toward the set point.
Each of these components is illustrated in Figure 10.7.210.7.2. The diagram on the left is a general model showing how the components interact to maintain homeostasis. The diagram on the right shows the example of body temperature. From the diagrams, you can see that maintaining homeostasis involves feedback, which is data that feeds back to control a response. Feedback may be negative, as in the example below, or positive. All the feedback mechanisms that maintain homeostasis use negative feedback. Biological examples of positive feedback are much less common.
Negative Feedback
In a negative feedback loop, feedback serves to reduce an excessive response and keep a variable within the normal range. Examples of processes controlled by negative feedback include body temperature regulation and control of blood glucose.
Body Temperature
Body temperature regulation involves negative feedback whether it lowers the temperature or raises it (Figure 10.7.310.7.3).
Cooling Down
The human body’s temperature regulatory center is the hypothalamus in the brain. When the hypothalamus receives data from sensors in the skin and brain that body temperature is higher than the set point, it sets into motion the following responses:
- Blood vessels in the skin dilate (vasodilation) to allow more blood from the warm body core to flow close to the surface of the body, so heat can be radiated into the environment.
- As blood flow to the skin increases, sweat glands in the skin are activated to increase their output of sweat (diaphoresis). When the sweat evaporates from the skin surface into the surrounding air, it takes the heat with it.
- Breathing becomes deeper, and the person may breathe through the mouth instead of the nasal passages. This increases heat loss from the lungs.

Heating Up
When the brain’s temperature regulatory center receives data that body temperature is lower than the set point, it sets into motion the following responses:
- Blood vessels in the skin contract (vasoconstriction) to prevent blood from flowing close to the surface of the body. This reduces heat loss from the surface.
- As the temperature falls lower, random signals to skeletal muscles are triggered, causing them to contract. This causes shivering, which generates a small amount of heat.
- The thyroid gland may be stimulated by the brain (via the pituitary gland) to secrete more thyroid hormone. This hormone increases metabolic activity and heat production in cells throughout the body.
- The adrenal glands may also be stimulated to secrete the hormone adrenaline. This hormone causes the breakdown of glycogen (the carbohydrate used for energy storage in animals) to glucose, which can be used as an energy source. This catabolic chemical process is exothermic, or heat producing.
Blood Glucose
In the control of the blood glucose level, certain endocrine cells in the pancreas called alpha and beta cells, detect the level of glucose in the blood. Then they respond appropriately to keep the level of blood glucose within the normal range.
- If the blood glucose level rises above the normal range, pancreatic beta cells release the hormone insulin into the bloodstream. Insulin signals cells to take up the excess glucose from the blood until the level of blood glucose decreases to the normal range.
- If the blood glucose level falls below the normal range, pancreatic alpha cells release the hormone glucagon into the bloodstream. Glucagon signals cells to break down stored glycogen to glucose and release the glucose into the blood until the level of blood glucose increases to the normal range.
Positive Feedback
In a positive feedback loop, feedback serves to intensify a response until an endpoint is reached. Examples of processes controlled by positive feedback in the human body include blood clotting and childbirth.
Blood Clotting
When a wound causes bleeding, the body responds with a positive feedback loop to clot the blood and stop blood loss. Substances released by the injured blood vessel wall begin the process of blood clotting. Platelets in the blood start to cling to the injured site and release chemicals that attract additional platelets. As the platelets continue to amass, more of the chemicals are released and more platelets are attracted to the site of the clot. The positive feedback accelerates the process of clotting until the clot is large enough to stop the bleeding.
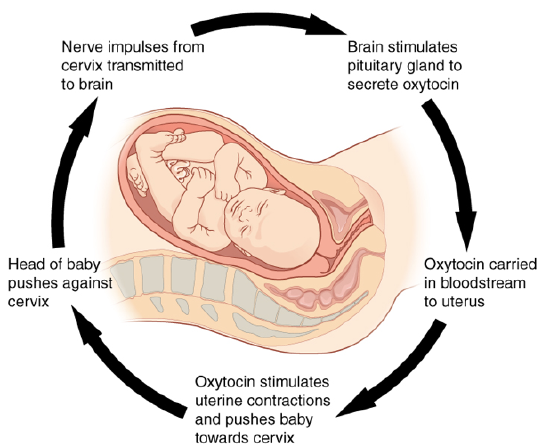
Childbirth
Figure 10.7.410.7.4 shows the positive feedback loop that controls childbirth. The process normally begins when the head of the infant pushes against the cervix. This stimulates nerve impulses, which travel from the cervix to the hypothalamus in the brain. In response, the hypothalamus sends the hormone oxytocin to the pituitary gland, which secretes it into the bloodstream so it can be carried to the uterus. Oxytocin stimulates uterine contractions, which push the baby harder against the cervix. In response, the cervix starts to dilate in preparation for the passage of the baby. This cycle of positive feedback continues, with increasing levels of oxytocin, stronger uterine contractions, and wider dilation of the cervix until the baby is pushed through the birth canal and out of the body. At that point, the cervix is no longer stimulated to send nerve impulses to the brain, and the entire process stops.
When Homeostasis Fails
Homeostatic mechanisms work continuously to maintain stable conditions in the human body. Sometimes, however, the mechanisms fail. When they do, homeostatic imbalance may result, in which cells may not get everything they need or toxic wastes may accumulate in the body. If homeostasis is not restored, the imbalance may lead to disease or even death. Diabetes is an example of a disease caused by homeostatic imbalance. In the case of diabetes, blood glucose levels are no longer regulated and may be dangerously high. Medical intervention can help restore homeostasis and possibly prevent permanent damage to the organism.
Normal aging may bring about a reduction in the efficiency of the body’s control systems. This makes the body more susceptible to disease. For example, older people may have a harder time regulating their body temperature. This is one reason they are more likely than younger people to develop serious heat-induced illnesses such as heat stroke.
Feature: My Human Body
Diabetes is diagnosed in people who have abnormally high levels of blood glucose after fasting for at least 12 hours. A fasting level of blood glucose below 100 is normal. A level between 100 and 125 places you in the pre-diabetes category, and a level higher than 125 results in a diagnosis of diabetes.
Of the two types of diabetes, type 2 diabetes is the most common, accounting for about 90 percent of all cases of diabetes in the United States. Type 2 diabetes typically starts after the age of 40. However, because of the dramatic increase in recent decades in obesity in younger people, the age at which type 2 diabetes is diagnosed has fallen. Even children are now being diagnosed with type 2 diabetes. Today, about 30 million Americans have type 2 diabetes, and another 90 million have pre-diabetes.
You are likely to have your blood glucose level tested during a routine medical exam. If your blood glucose level indicates that you have diabetes, it may come as a shock to you because you may not have any symptoms of the disease. You are not alone, because as many as one in four diabetics do not know they have the disease. Once the diagnosis of diabetes sinks in, you may be devastated by the news. Diabetes can lead to heart attacks, strokes, blindness, kidney failure, and loss of toes or feet. The risk of death in adults with diabetes is 50 percent greater than it is in adults without diabetes, and diabetes is the seventh leading cause of death of adults. In addition, controlling diabetes usually requires frequent blood glucose testing, watching what and when you eat, and taking medications or even insulin injections. All of this may seem overwhelming.
The good news is that changing your lifestyle may stop the progression of type 2 diabetes or even reverse it. By adopting healthier habits, you may be able to keep your blood glucose level within the normal range without medications or insulin. Here’s how:
- Lose weight. Any weight loss is beneficial. Losing as little as seven percent of your weight may be all that is needed to stop diabetes in its tracks. It is especially important to eliminate excess weight around your waist.
- Exercise regularly. You should try to exercise five days a week for at least 30 minutes. This will not only lower your blood sugar and help your insulin work better; it will also lower your blood pressure and improve your heart health. Another bonus of exercise is that it will help you lose weight by increasing your basal metabolic rate.
- Adopt a healthy diet. Decrease your consumption of refined carbohydrates such as sweets and sugary drinks. Increase your intake of fiber-rich foods such as fruits, vegetables, and whole grains. About a quarter of each meal should consist of high-protein foods, such as fish, chicken, dairy products, legumes, or nuts.
- Control stress. Stress can increase your blood glucose and also raise your blood pressure and risk of heart disease. When you feel stressed out, do breathing exercises or take a brisk walk or jog. Also, try to replace stressful thoughts with more calming ones.
- Establish a support system. Enlist the help and support of loved ones as well as medical professionals such as a nutritionist and diabetes educator. Having a support system will help ensure that you are on the path to wellness and that you can stick to your plan.
