Introduction
A definition of pain is provided by the International association for the Study of Pain (IASP) as follows:[1]
An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage
Pain is always subjective and everyone learns the use of this word through experiences related to injury in early life.
Pain is a sensation in a part or parts of the body. It can vary in intensity, quality, duration and pain can refer to other parts of the body. Pain is usually an unpleasant sensation and therefore it also has an emotional aspect. It is strongly linked to suffering.[2]
Even in the absence of tissue damage or any likely pathophysiological cause, people still report pain. This could happen for psychological reasons. In these cases, it is challenging to distinguish whether someone’s experience of pain arises from damaged tissue or not, as it can only be based upon the subjective report of such experience.[3]
In the following video, Karen D. Davis tries to explain why some people react to the same painful stimulus in different ways.
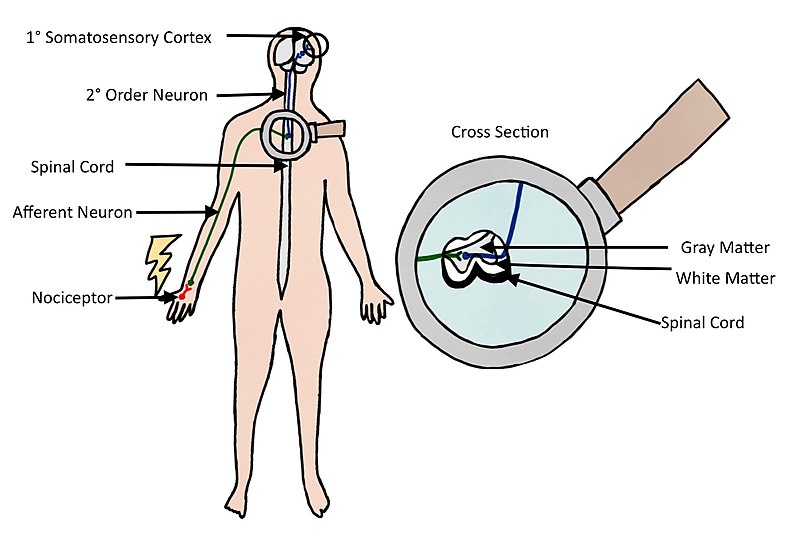
The Process of Feeling Pain
Pain is a physiological protective system. It is essential to warn, detect, and minimize contact with damaging stimuli.[5] Nerve endings and sensory receptors in the skin and tissues detect sensory stimuli. This can be thermal, mechanical or chemical stimuli (heat, cold, pressure, etc.). Nociceptors (from the Latin word nocere that means “to hurt”) are sensory receptors that respond to damaging or potentially damaging stimuli. With the stimulation of a nociceptor, a noxious stimulus is converted into electrical activity in the peripheral terminals of nociceptor sensory fibres. This is called transduction. The stimulus is carried to the spinal cord (central nervous system) through a process called conduction. The nociceptive nerve fibres terminate and the synaptic transfer and modulation of input from one neuron to another take place. This is called transmission. The neurons in the dorsal horn of the spinal cord transfer nociceptive input to the brainstem, hypothalamus, thalamus and brain cortex. In the brain perception of the experience occurs. This is a subjective process. Only then does the brain create pain as output after processing the stimuli. It is important to underline that activity induced in the nociceptive pathways by a noxious stimulus does not always lead to pain. Nociceptors can be stimulated by potentially damaging stimuli as well as actual damaging stimuli. Only when the brain has processed the stimulus, will it lead to a response of pain or not. Pain is always the output of a widely distributed neural network in the brain rather than one coming directly by sensory input evoked by injury, inflammation or other pathology[6].
Pain Classification
Based on the works of Woolf[5], this is a useful way of classifying pain:
- Nociceptive pain. This kind of pain is concerned with the sensing of noxious stimuli. It is a signal of impending or actual tissue damage and is a high-threshold pain only activated in the presence of intense stimuli. It has a protective role requiring immediate attention and responses (i.e. withdrawal reflex). For example, touching something too hot, cold or sharp
- Inflammatory pain. This second kind of pain is important to promote healing and protection of injured tissues. It increases sensory sensitivity through pain hypersensitivity and tenderness. Thus normally innocuous stimuli now elicit pain. It creates an environment which suggests avoidance of movement, contact and stress of the injured body parts. This, in turn, assists in the healing of the injured body part. Inflammatory pain is caused by activation of the immune system that causes inflammation after tissue injury or infection. This type of pain can be seen as a protective mechanism, However, it still needs to be reduced in patients with ongoing inflammation, as with rheumatoid arthritis or in cases of severe or extensive injury.
- Pathological pain. This type of pain is not protective, but rather maladaptive. It is not connected to tissue damage but results from abnormal functioning of the nervous system. To note, this is a low-threshold pain. Pathological pain can occur after damage to the nervous system or even when there is no damage or inflammation, It is largely the consequence of amplified sensory signals in the central nervous system. Conditions that cause this type of pain include fibromyalgia, irritable bowel syndrome, tension-type headache, temporomandibular joint disease etc. Usually, the pain is substantial without any noxious stimulus and minimal or even no peripheral inflammation.
Acute pain is caused by noxious stimuli and is mediated by nociception. It has an early onset and serves to prevent tissue damage. This is why this type of pain is defined as adaptive, it helps to survive and to heal[2]
Chronic pain is pain continuing beyond 3 months, or after healing is complete[3]. It may arise as a consequence of tissue damage or inflammation or have no identified cause. Chronic pain is a complex condition embracing physical, social and psychological factors, consequently leading to disability, loss of independence and poor quality of life.[7]
In the past, psychological and physiological (or pathophysiological) factors were considered as separate components in a dualistic point of view. Later, the recognition that psychosocial factors, such as emotional stress and fear, could impact the reporting of symptoms, medical disorders, and response to treatment lead to the development of the biopsychosocial model of pain[8].
The bio part represents the pathophysiology of the disease or the mechanism of injury, and the relative nociception processes, it considers the physiological aspects of the pain experience.
The psychosocial part involves both emotion (the more immediate reaction to nociception and is more midbrain based) and cognition (which attach meaning to the emotional experience). These could trigger additional emotional reactions and thereby amplify the experience of pain, thus perpetuating a vicious circle of nociception, pain, distress, and disability.[8]
It could be said that psychological factors, such as fear and anxiety, play an important role in the development of chronic pain. [8]
Psychological Factors in Pain
Anxiety
Health anxious individuals form dysfunctional assumptions and beliefs about pain and other symptoms. This can be disease based and based on past experiences. They will have a tendency to misinterpret somatic information as catastrophic and personally threatening. Some studies report an increase in pain correlated with increased levels of anxiety.[9] Clinically, anxiety can compromise treatments as practitioners can expect to see catastrophization play a big role in these patients’ report and they could report greater pain during activities. Thus, there is a need to target attentional focus and interpretation of sensations among health anxious clients.
Depression
There is strong evidence of established comorbidity of pain and depression.[10] Furthermore, when patients with pain have comorbid depression, they could experience greater pain, have a worse prognosis, and more functional disability. Pain and depression are linked by neurobiological, cognitive, affective and behavioural factors. Thus, the optimal treatment approach for comorbid pain and depression should simultaneously address both physical and psychological symptoms.
Expectation
When an individual expects to experience pain, the perceived pain may vary based upon the types of cues received (i.e. a cue may indicate a more intense or damaging stimulus, then more intense pain is perceived and vice versa). Cues of an impending treatment could also decrease pain, for example, the process of taking an analgesic, usually decreases pain.[9] Thus, expectation is thought to play a big role in the placebo effect.
Attention and Distraction
There is strong evidence that attention (and distraction) is highly effective in modulating the pain experience and demonstrate how cognitive processes can interfere with pain perception. When a person is distracted with a cognitive task pain is perceived as less intense, even in chronic pain patients. On the other hand, pain increases when it is the focus of attention. Functional brain imaging and neurophysiological studies have shown that attention and cognitive distraction-related modulations of nociceptive driven activations take place in various pain-sensitive cortical and subcortical brain regions, accompanied by concordant changes in pain perception.[11]
Fear
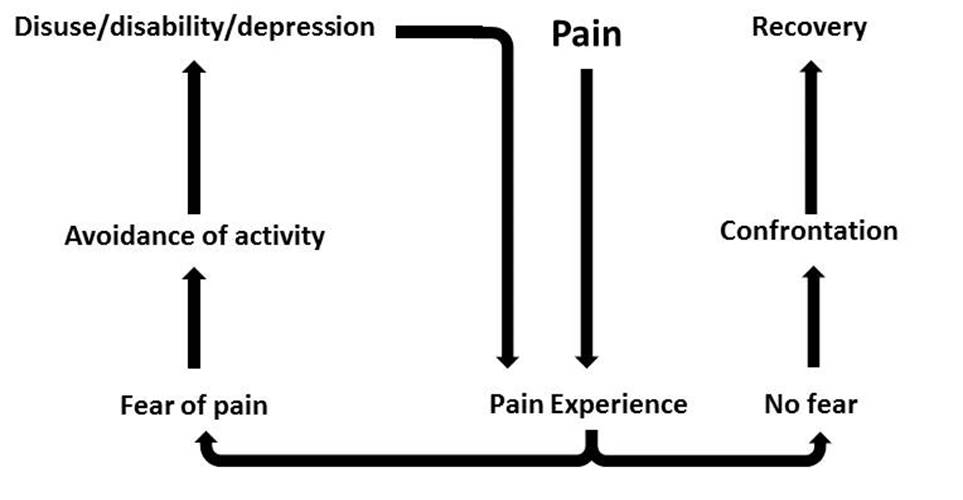
Pain-related fear is a general term to describe several forms of fear with respect to pain. Fear of pain can be directed toward the occurrence or continuation of pain, toward physical activity, or toward (re)-injury or physical harm. Fear toward physical activity is also known as kinesiophobia. It can be defined as “an excessive, irrational, and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or re-injury”.[12] If pain, possibly caused by an injury, is interpreted as threatening, pain-related fear will lead to avoidance behaviours and hypervigilance to bodily sensations. This, in turn, will lead to disability, disuse and depression. This will maintain the pain experience, thereby fueling the vicious circle of increasing fear and avoidance.
Social and Cultural Factors in Pain
Culturally-specific attitudes and beliefs about pain can influence the manner in which individuals view and respond both to their own pain and to the pain of others. Cultural factors related to the pain experience include pain expression, pain language, lay remedies for pain, social roles, expectations and perceptions of the medical care system.[13]
Another psychosocial factor that may influence differences in pain responses is the gender role. Individuals who considered themselves more masculine and less sensitive to pain have been shown to have higher pain thresholds and tolerances.[14]
Socioeconomic factors (e.g. lower levels of education and income) seem to correlate with a higher incidence of chronic pain diagnosis and pain perception level.[15]
Clinical Implications
There is a direct relationship between physiological, psychological, and social factors in any individual’s pain experience.[9] This can perpetuate or may even worsen the clinical presentation.[8]
- There is a need for sound knowledge of how these factors interact. Clinicians must have the knowledge of not only anatomy, biomechanics and pathophysiology etc., but also of diagnostic tools, outcome measures, tissue healing, peripheral and central sensitisation, and any psychological and social factors that could influence the patient’s perception of pain.[9]
- Patients should be helped and taught to base their reasoning about their condition and their pain on similar information as mentioned in the previous point. It is important to teach patients about more modern pain neuroscience in a way that they could understand. This could help them to change their attitudes and beliefs about pain and decrease chronic pain and disability.[9]
- Targeting psychosocial factors should be a key component of any pain intervention. Treatment programs must be individually-tailored in order to specifically address the patients’ attitudes and beliefs to improve treatment adherence and outcome. Treatments should also be targeted at the different pain mechanisms responsible. [5]
Candela Citations
- Multidimensional Nature of Pain. Located at: https://www.physio-pedia.com/Multidimensional_Nature_of_Pain. License: CC BY-SA: Attribution-ShareAlike