Gastrointestinal tract, also called digestive tract or alimentary canal, pathway by which food enters the body and solid wastes are expelled. The gastrointestinal tract includes the mouth, pharynx, esophagus, stomach, small intestine, large intestine, and anus. See digestion.
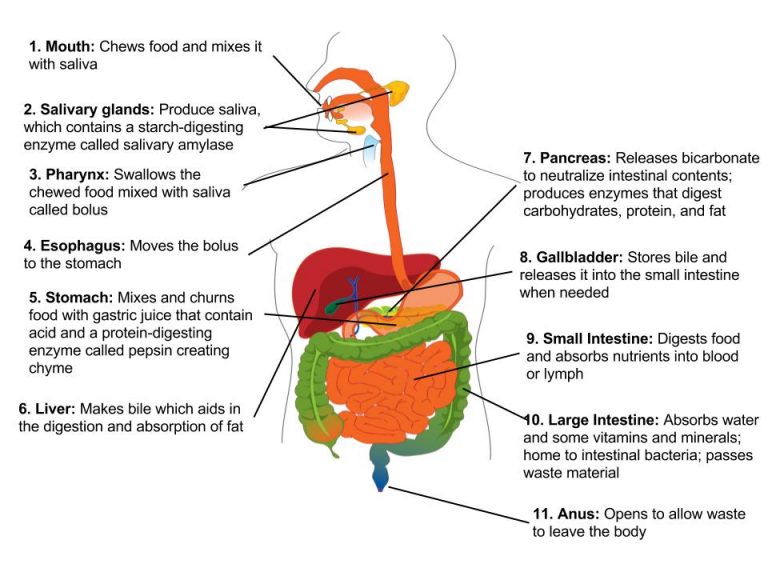
Figure 1: Digestive system organs and functions – overview.
The Oral Cavity or Mouth:
The oral cavity, or mouth, is the point of entry of food into the digestive system. The cheeks, tongue, and palate frame the mouth, which is also called the oral cavity (or buccal cavity). The arched shape of the roof of your mouth is called the palate. If you run your tongue along the roof of your mouth, the front part is the hard palate, and at the back, the roof becomes fleshier. This part of the palate, known as the soft palate. A fleshy bead of tissue called the uvula drops down from the center of the posterior edge of the soft palate. Although some have suggested that the uvula is a vestigial organ, it serves an important purpose. When you swallow, the soft palate and uvula move upward, helping to keep foods and liquid from entering the nasal cavity. Unfortunately, it can also contribute to the sound produced by snoring. Two muscular folds extend downward from the soft palate, on either side of the uvula. Between these two arches are the palatine tonsils, clusters of lymphoid tissue that protect the pharynx. The lingual tonsils are located at the base of the tongue. These glands make antibodies that help fight infection. Tonsillitis means that your tonsils are inflamed. Both bacteria and viruses can cause tonsillitis.

Figure 2: Oral cavity
The Tongue
The tongue is a workhorse, facilitating ingestion, mechanical digestion, chemical digestion (lingual lipase), sensation (of taste, texture, and temperature of food), swallowing, and vocalization. The tongue perform three important digestive functions in the mouth:
- Position food for optimal chewing
- Gather food into a bolus (rounded mass)
- Position food so it can be swallowed
A fold of mucous membrane on the underside of the tongue, the lingual frenulum, tethers the tongue to the floor of the mouth. People with the congenital anomaly ankyloglossia, also known by the non-medical term “tongue tie,” have a lingual frenulum that is too short or otherwise malformed. Severe ankyloglossia can impair speech and must be corrected with surgery.
The Teeth
The teeth, or dentes (singular = dens), are organs similar to bones that you use to tear, grind, and otherwise mechanically break down food. During the course of your lifetime, you have two sets of teeth (one set of teeth is a dentition). Your 20 deciduous teeth, or baby teeth, first begin to appear at about 6 months of age. Between approximately age 6 and 12, these teeth are replaced by 32 permanent teeth. Moving from the center of the mouth toward the side, these are as follows:
- The eight incisors, four top and four bottom, are the sharp front teeth you use for biting into food.
- The four cuspids (or canines) flank the incisors and have a pointed edge (cusp) to tear up food. These fang-like teeth are superb for piercing tough or fleshy foods.
- Posterior to the cuspids are the eight premolars (or bicuspids), which have an overall flatter shape with two rounded cusps useful for mashing foods.
- The most posterior and largest are the 12 molars, which have several pointed cusps used to crush food so it is ready for swallowing. The third members of each set of three molars, top and bottom, are commonly referred to as the wisdom teeth, because their eruption is commonly delayed until early adulthood. It is not uncommon for wisdom teeth to fail to erupt; that is, they remain impacted. In these cases, the teeth are typically removed by orthodontic surgery.
Anatomy of a Tooth: The teeth are secured in the alveolar processes (sockets) of the maxilla and the mandible. Gingivae (commonly called the gums) are soft tissues that line the alveolar processes and surround the necks of the teeth.

Figure 3: This longitudinal section through a molar in its alveolar socket shows the relationships between enamel, dentin, and pulp.
The two main parts of a tooth are the crown, which is the portion projecting above the gum line, and the root, which is embedded within the maxilla and mandible. Both parts contain an inner pulp cavity, containing loose connective tissue through which run nerves and blood vessels. The region of the pulp cavity that runs through the root of the tooth is called the root canal. Surrounding the pulp cavity is dentin, a bone-like tissue. In the root of each tooth, the dentin is covered by an even harder bone-like layer called cementum. In the crown of each tooth, the dentin is covered by an outer layer of enamel, the hardest substance in the body.
Although enamel protects the underlying dentin and pulp cavity, it is still nonetheless susceptible to mechanical and chemical erosion, or what is known as tooth decay. The most common form, dental caries (cavities) develops when colonies of bacteria feeding on sugars in the mouth release acids that cause soft tissue inflammation and degradation of the calcium crystals of the enamel.
PeriONDONTAL DISEASES / Gum diseases

Figure 4:: Advanced periodontal disease
The word periodontal means “around the tooth.” Periodontal diseases, also called gum diseases, are serious bacterial infections that attack the gums and the surrounding tissues. If it’s left untreated, the disease will continue and the underlying bone around the teeth will dissolve and will no longer be able to hold the teeth in place.
Gingivitis. This is the mildest form of periodontal disease. The gums are likely to become red, swollen, and tender. They may bleed easily during daily cleanings and flossing.
Moderate to advanced periodontitis. This most advanced stage of gum disease shows significant bone loss, deepening of periodontal pockets, and possibly receding gums surrounding the teeth. Teeth may loosen and need to be extracted.
The Salivary Glands
Many small salivary glands are housed within the mucous membranes of the mouth and tongue. These minor exocrine glands are constantly secreting saliva, either directly into the oral cavity or indirectly through ducts, even while you sleep.

Figure 5:. Digestion of food begins in the (a) oral cavity. Food is masticated by teeth and moistened by saliva secreted from the (b) salivary glands. Enzymes in the saliva begin to digest starches and fats. With the help of the tongue, the resulting bolus is moved into the esophagus by swallowing. (credit: modification of work by the National Cancer Institute)
The Major Salivary Glands
- The submandibular glands, which are in the floor of the mouth, secrete saliva into the mouth through the submandibular ducts.
- The sublingual glands, which lie below the tongue, use the lesser sublingual ducts to secrete saliva into the oral cavity.
- The parotid glands lie between the skin and the masseter muscle, near the ears
Saliva: The extensive chemical process of digestion begins in the mouth. As food is being chewed, saliva, produced by the salivary glands, mixes with the food. Saliva is a watery substance produced in the mouths of many animals. Saliva contains mucus that moistens food and buffers the pH of the food. Saliva also contains lysozymes, which have antibacterial action to reduce tooth decay by inhibiting growth of some bacteria. Saliva also contains an enzyme called salivary amylase that begins the process of converting starches in the food into a disaccharide called maltose. Another enzyme called lipase is produced by the cells in the tongue. Lipases are a class of enzymes that can break down triglycerides- fats. The chewing and wetting action provided by the teeth and saliva prepare the food into a mass called the bolus for swallowing. The tongue helps in swallowing—moving the bolus from the mouth into the pharynx.
HOMEOSTATIC IMBALANCES : Mumps
The Parotid Glands: Mumps
Infections of the nasal passages and pharynx can attack any salivary gland. The parotid glands are the usual site of infection with the virus that causes mumps (paramyxovirus). Mumps manifests by enlargement and inflammation of the parotid glands, causing a characteristic swelling between the ears and the jaw. Symptoms include fever and throat pain, which can be severe when swallowing acidic substances such as orange juice.
In about one-third of men who are past puberty, mumps also causes testicular inflammation, typically affecting only one testis and rarely resulting in sterility. With the increasing use and effectiveness of mumps vaccines, the incidence of mumps has decreased dramatically.
The pharynx:

Figure 6: The pharynx, which runs from the nostrils to the esophagus and the larynx.
The pharynx (throat) is involved in both digestion and respiration. It receives food and air from the mouth, and air from the nasal cavities. The pharynx located in throat, connects mouth to the esophagus. Pharynx has three subdivisions. The most superior, the nasopharynx, is involved only in breathing and speech. The other two subdivisions, the oropharynx and the laryngopharynx, are used for both breathing and digestion.
Pharynx opens to two passageways:
- the trachea, which leads to the lungs, ( air way) and
- the esophagus, which leads to the stomach.
The trachea has an opening called the glottis, which is covered by a cartilaginous flap called the epiglottis. When swallowing, the epiglottis closes the glottis and food passes into the esophagus and not the trachea. This arrangement allows food to be kept out of the trachea. When the food “goes down the wrong way,” it goes into the trachea. When food enters the trachea, the reaction is to cough, which usually forces the food up and out of the trachea, and back into the pharynx.
Esophagus

Figure 7. The esophagus transfers food from the mouth to the stomach through peristaltic movements.
The esophagus is a tubular organ that connects the mouth to the stomach. The chewed and softened food passes through the esophagus after being swallowed. The smooth muscles of the esophagus undergo a series of wave like movements called peristalsis that push the food toward the stomach. The peristalsis wave is unidirectional—it moves food from the mouth to the stomach.
A ring-like muscle called a sphincter forms valves in the digestive system. The gastro-esophageal sphincter is located at the stomach end of the esophagus. In response to swallowing and the pressure exerted by the bolus of food, this sphincter opens, and the bolus enters the stomach. When there is no swallowing action, this sphincter is shut and prevents the contents of the stomach from traveling up the esophagus. When the lower esophageal sphincter does not completely close, the stomach’s contents can reflux (that is, back up into the esophagus), causing heartburn or gastroesophageal reflux disease (GERD)..
Figure 8: Layers of stomach lining
The Stomach
The stomach is a J-shaped saclike organ in the upper abdomen. The stomach is much like a bag which store food and secretes gastric digestive juices. The wall of the stomach is made of the same four layers as most of the rest of the alimentary canal. In addition to the typical circular and longitudinal smooth muscle layers, the muscularis has an inner oblique smooth muscle layer. As a result, in addition to moving food through the canal, the stomach can vigorously churn food, mechanically breaking it down into smaller particles. In the absence of food, the stomach deflates inward, and its mucosa and submucosa fall into a large fold called a ruga.
The pH in the stomach is between 1.5 and 2.5. This highly acidic environment is required for the chemical breakdown of food and the extraction of nutrients.A large part of digestion occurs in the stomach.

Figure 9: The stomach wall showing wall layers, gastric pit and gastric glands.(one gland is shown enlarged on the right)
The stomach wall is adapted for the functions of the stomach. In the epithelium, gastric pits lead to gastric glands that secrete gastric juice. The gastric glands contain different types of cells that secrete a variety of enzymes, including hydrochloride acid (HCl), which activates the protein-digesting enzyme pepsin.
- Parietal cells— produce both hydrochloric acid (HCl) and intrinsic factor. HCl is responsible for the high acidity (pH 1.5 to 3.5) of the stomach contents and is needed to activate the protein-digesting enzyme, pepsin. The acidity also kills much of the bacteria you ingest with food and helps to denature proteins, making them more available for enzymatic digestion. Intrinsic factor is a glycoprotein necessary for the absorption of vitamin B12 in the small intestine. The parietal cells are capable of creating a very acidic pH of 2.0 within the stomach.
- Chief cells—Located primarily in the basal regions of gastric glands are chief cells, which secrete pepsinogen, the inactive proenzyme form of pepsin. HCl is necessary for the conversion of pepsinogen to pepsin.
- Mucous neck cells—secrete thin, acidic mucus that is much different from the mucus secreted by the goblet cells of the surface epithelium. The role of this mucus is not currently known.
- Enteroendocrine cells— secrete various hormones – include gastrin,
The combination of all of the stomach secretions is known as gastric juice. Food enters the stomach and combines with gastric juice to form a pasty substance called chyme. Chyme then leaves the stomach by way of the pyloric sphincter and enters the duodenum.
The Mucosal Barrier: The mucosa of the stomach is exposed to the highly corrosive acidity of gastric juice. Gastric enzymes that can digest protein can also digest the stomach itself. The stomach is protected from self-digestion by the mucosal barrier. This barrier has several components. First, the stomach wall is covered by a thick coating of bicarbonate-rich mucus. This mucus forms a physical barrier, and its bicarbonate ions neutralize acid. Second, the epithelial cells of the stomach’s mucosa meet at tight junctions, which block gastric juice from penetrating the underlying tissue layers. Finally, stem cells located where gastric glands join the gastric pits quickly replace damaged epithelial mucosal cells, when the epithelial cells are shed. In fact, the surface epithelium of the stomach is completely replaced every 3 to 6 days.
HOMEOSTATIC IMBALANCES: ULCERS
As effective as the mucosal barrier is, it is not a “fail-safe” mechanism. Sometimes, gastric juice eats away at the superficial lining of the stomach mucosa, creating erosions, which mostly heal on their own. Deeper and larger erosions are called ulcers.

Figure 10: Ulcer-causing Bacterium (H.Pylori) Crossing Mucus Layer of Stomach
Why does the mucosal barrier break down? A number of factors can interfere with its ability to protect the stomach lining. The majority of all ulcers are caused by either excessive intake of non-steroidal anti-inflammatory drugs (NSAIDs), including aspirin, or Helicobacter pylori infection.
Antacids help relieve symptoms of ulcers such as “burning” pain and indigestion. When ulcers are caused by NSAID use, switching to other classes of pain relievers allows healing. When caused by H. pylori infection, antibiotics are effective.
A potential complication of ulcers is perforation: Perforated ulcers create a hole in the stomach wall, resulting in peritonitis (inflammation of the peritoneum). These ulcers must be repaired surgically.
Small Intestine
The small intestine is a long muscular tube of about 20 feet long and about an inch in diameter. Chyme moves from the stomach to the small intestine. The small intestine is the organ where the digestion of protein, fats, and carbohydrates is completed and absorb most of the nutrients from what we eat and drink.
Small Intestine – Structure
The coiled tube of the small intestine is subdivided into three regions. From proximal (at the stomach) to distal, these are the Duodenum, Jejunum, and Ileum.
- The shortest region is the 25.4-cm (10-in) duodenum, which begins at the pyloric sphincter and makes a C-shaped curve and join the jejunum.. Digestive juices from the pancreas, liver, and gallbladder enter the duodenum. Bile is produced in the liver and stored and concentrated in the gallbladder. Bile contains bile salts which emulsify lipids while the pancreas produces enzymes that catabolize starches, disaccharides, proteins, and fats. These digestive juices break down the food particles in the chyme into glucose, triglycerides, and amino acids. Some chemical digestion of food takes place in the duodenum. Absorption of fatty acids also takes place in the duodenum.

Figure 11. The three regions of the small intestine are the duodenum, jejunum, and ileum
- The jejunum is about 0.9 meters (3 feet) long (in life) and runs from the duodenum to the ileum. Here, hydrolysis of nutrients is continued while most of the carbohydrates and amino acids are absorbed through the intestinal lining. The bulk of chemical digestion and nutrient absorption occurs in the jejunum.
- The ileum is the longest part of the small intestine, measuring about 1.8 meters (6 feet) in length. The ileum joins the cecum, the first portion of the large intestine, at the ileocecal sphincter (or valve). The undigested food is sent to the colon from the ileum via peristaltic movements of the muscle. The vermiform, “worm-like,” appendix is located at the ileocecal valve. The appendix of humans secretes no enzymes and has an insignificant role in immunity.
Histology
The wall of the small intestine is composed of the same four layers typically present in the alimentary system. The small intestine has a highly folded inner surface containing finger-like projections called the villi. The apical surface of each villus has many microscopic projections called microvilli. Although their small size makes it difficult to see each microvillus, their combined microscopic appearance suggests a mass of bristles, which is termed the brush border. These structures are lined with epithelial cells on the luminal side and allow for the nutrients to be absorbed from the digested food and absorbed into the blood stream on the other side. The villi and microvilli, with their many folds, increase the surface area of the intestine and increase absorption efficiency of the nutrients. Absorbed nutrients in the blood are carried into the blood in hepatic portal vein, which leads to the liver. There, the liver regulates the distribution of nutrients to the rest of the body and removes toxic substances, including drugs, alcohol, and some pathogens.
ART CONNECTION

Figure 12. Villi are folds on the small intestine lining that increase the surface area to facilitate the absorption of nutrients.
Which of the following statements about the small intestine is false?
- Absorptive cells that line the small intestine have microvilli, small projections that increase surface area and aid in the absorption of food.
- The inside of the small intestine has many folds, called villi.
- Microvilli are lined with blood vessels as well as lymphatic vessels.
- The inside of the small intestine is called the lumen.
Large Intestine

Figure 13. Structure of the large intestine
The large intestine, illustrated in Figure 13, reabsorbs the water from the undigested food material and processes the waste material. The human large intestine is much smaller in length compared to the small intestine but larger in diameter. It has three parts: the cecum, the colon, and the rectum. The cecum joins the ileum to the colon and is the receiving pouch for the waste matter. The colon can be divided into four regions, the ascending colon, the transverse colon, the descending colon and the sigmoid colon. The main functions of the colon are to extract the water and mineral salts from undigested food, and to store waste material. The colon is home to many bacteria or “intestinal flora” that aid in the digestive processes.
Bacterial Flora
Most bacteria that enter the alimentary canal are killed by lysozyme, defensins, HCl, or protein-digesting enzymes. However, trillions of bacteria live within the large intestine and are referred to as the bacterial flora. Most of the more than 700 species of these bacteria are nonpathogenic commensal organisms that cause no harm as long as they stay in the gut lumen. In fact, many facilitate chemical digestion and absorption, and some synthesize certain vitamins, mainly biotin, pantothenic acid, and vitamin K. Fecal transplantation (or bacteriotherapy) is the transfer of stool from a healthy donor into the gastrointestinal tract for the purpose of treating recurrent C. difficile colitis. When antibiotics kill off too many “good” bacteria in the digestive tract, fecal transplants can help replenish bacterial balance.
HOMEOSTATIC IMBALANCES: COLORECTAL CANCER
Each year, approximately 140,000 Americans are diagnosed with colorectal cancer, and another 49,000 die from it, making it one of the most deadly malignancies. People with a family history of colorectal cancer are at increased risk. Smoking, excessive alcohol consumption, and a diet high in animal fat and protein also increase the risk. Despite popular opinion to the contrary, studies support the conclusion that dietary fiber and calcium do not reduce the risk of colorectal cancer.
Colorectal cancer may be signaled by constipation or diarrhea, cramping, abdominal pain, and rectal bleeding. Bleeding from the rectum may be either obvious or occult (hidden in feces). Since most colon cancers arise from benign mucosal growths called polyps, cancer prevention is focused on identifying these polyps. The colonoscopy is both diagnostic and therapeutic. Colonoscopy not only allows identification of precancerous polyps, the procedure also enables them to be removed before they become malignant. Screening for fecal occult blood tests and colonoscopy is recommended for those over 50 years of age.
Rectum and Anus
The rectum is the terminal end of the large intestine, as shown in Figure 13. The primary role of the rectum is to store the feces until defecation. The feces are propelled using peristaltic movements during elimination. The anus is an opening at the far-end of the digestive tract and is the exit point for the waste material.
The small intestine absorbs about 90 percent of the water you ingest (either as liquid or within solid food). The large intestine absorbs most of the remaining water, a process that converts the liquid chyme residue into semisolid feces (“stool”). Feces is composed of undigested food residues, unabsorbed digested substances, millions of bacteria, old epithelial cells from the GI mucosa, inorganic salts, and enough water to let it pass smoothly out of the body.
Feces are eliminated through contractions of the rectal muscles. You help this process by a voluntary procedure called Valsalva’s maneuver, in which you increase intra-abdominal pressure by contracting your diaphragm and abdominal wall muscles, and closing your glottis.
iRRITABLE BOWEL SYNDROME – IBS
Irritable bowel syndrome (IBS) is characterized by abdominal discomfort associated with altered bowel movements and change in your bowel habits. IBS cause abdominal discomfort in different ways, such as sharp pain, cramping, bloating, distention, fullness or even burning. IBS may be triggered by eating specific foods, following a meal, emotional stress, constipation or diarrhea. Many symptoms are related to hypersensitivity of the nerves found in the wall of the gastrointestinal tract.
Accessory Organs
Each accessory digestive organ aids in the breakdown of food. Within the mouth, the teeth and tongue begin mechanical digestion. Other accessory organs add secretions (enzymes) that catabolize food into nutrients.

Figure:14 Accessory organs of digestive system
Accessory organs include salivary glands, the liver, the pancreas, and the gallbladder.
- 1. Salivary glands: There are three major salivary glands that secrete saliva into the oral cavity —the parotid, the submandibular, and the sublingual. Saliva contains mucus that moistens food and buffers the pH of the food.
- 2. The Liver: The liver is the largest gland in the body, weighing about three pounds in an adult. It is the largest internal organ in humans and it plays a very important role in digestion of fats and detoxifying blood. The liver lies inferior to the diaphragm in the right upper quadrant of the abdominal cavity and receives protection from the surrounding ribs. The liver is divided into two primary lobes: a large right lobe and a much smaller left lobe. The lobes are further divided into lobules by blood vessels and connective tissue. The liver performs many functions and is considered a vital organ.
Liver functions include:
Detoxifying the blood, producing bile, (a digestive juice that is required for the breakdown of fatty components of the food in the duodenum.), metabolism of carbohydrates, fats and proteins, storing iron, blood and vitamins, recycling red blood cells and producing plasma proteins.
DISORDERS OF THE LIVER: Cirrhosis
Cirrhosis is when scar tissue replaces healthy liver tissue. This stops the liver from working normally.Cirrhosis is a long-term (chronic) liver disease. The damage to your liver builds up over time.The most common causes of cirrhosis are:
- Hepatitis: inflammation of the liver. Liver inflammation can be caused by several viruses (viral hepatitis), chemicals, drugs, alcohol, certain genetic disorders or by an overactive immune system that mistakenly attacks the liver, called autoimmune hepatitis. Depending on its course, hepatitis can be acute, which flares up suddenly and then goes away, or chronic, which is a long-term condition usually producing more subtle symptoms and progressive liver damage.
- Nonalcoholic fatty liver disease (this happens from metabolic syndrome and is caused by conditions such as obesity, high cholesterol and triglycerides, and high blood pressure)
- What is Hepatitis C and Why Should You Care?
-
https://www.youtube.com/watch?v=IxCelFhuhQo
Bile : composition and function.
Bile is a mixture secreted by the liver to accomplish the emulsification of lipids in the small intestine. Recall that lipids are hydrophobic, that is, they do not dissolve in water. Thus, before they can be digested in the watery environment of the small intestine, large lipid globules must be broken down into smaller lipid globules, a process called emulsification.
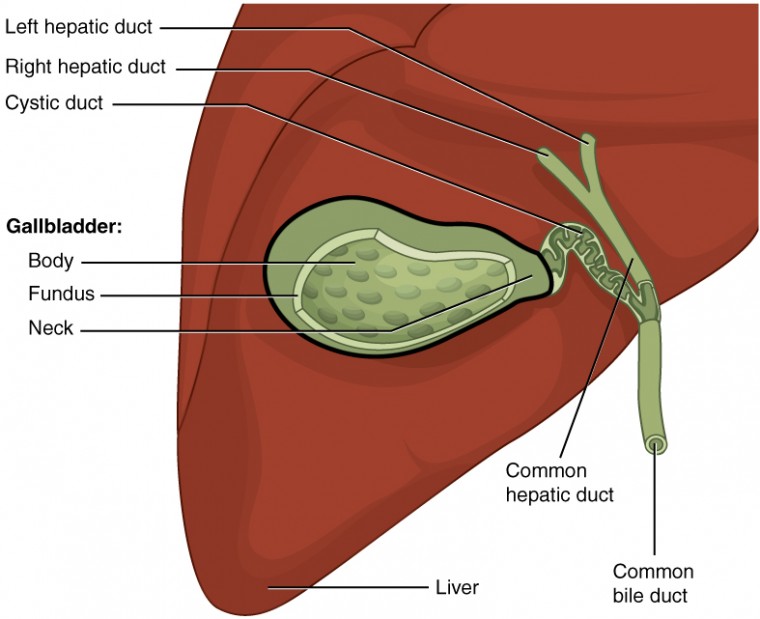
Figure 15. The gallbladder stores and concentrates bile, and releases it into the two-way cystic duct when it is needed by the small intestine.
Hepatocytes (cells of liver) secrete about one liter of bile each day. A yellow-brown or yellow-green alkaline solution (pH 7.6 to 8.6), bile is a mixture of water, bile salts, bile pigments, phospholipids (such as lecithin), electrolytes, cholesterol, and triglycerides. The components most critical to emulsification are bile salts and phospholipids, which have a nonpolar (hydrophobic) region as well as a polar (hydrophilic) region. The hydrophobic region interacts with the large lipid molecules, whereas the hydrophilic region interacts with the watery chyme in the intestine. This results in the large lipid globules being pulled apart into many tiny lipid fragments of about 1 µm in diameter. This change dramatically increases the surface area available for lipid-digesting enzyme activity. This is the same way dish soap works on fats mixed with water. Bile salts act as emulsifying agents, so they are also important for the absorption of digested lipids.
Bilirubin, the main bile pigment, is a waste product produced when the spleen removes old or damaged red blood cells from the circulation. Bilirubin is eventually transformed by intestinal bacteria into stercobilin, a brown pigment that gives your stool its characteristic color!
Gallbladder stores and releases bile: The gallbladder is 8–10 cm (~3–4 in) long and is nested in the right lobe of the liver. The liver secretes bile which is stored in the gallbladder. This muscular sac stores, concentrates, and, when stimulated, propels the bile into the duodenum via the common bile duct. When chyme containing fatty acids enters the duodenum, the bile is secreted from the gallbladder into the duodenum.
Pancreas
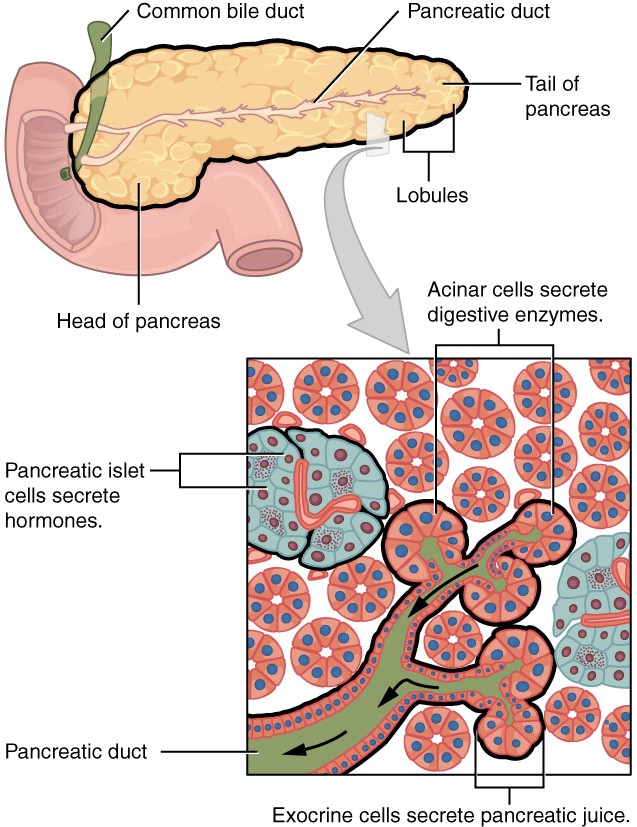
Figure 16. The pancreas has a head, a body, and a tail. It delivers pancreatic juice to the duodenum through the pancreatic duct.
The pancreas is another important gland that secretes digestive juices. The pancreas produces over a liter of pancreatic juice each day. Unlike bile, it is clear and composed mostly of water along with some salts, sodium bicarbonate, and several digestive enzymes.
- Sodium bicarbonate is responsible for the slight alkalinity of pancreatic juice (pH 7.1 to 8.2), which serves to buffer the acidic gastric juice in chyme, inactivate pepsin from the stomach, and create an optimal environment for the activity of pH-sensitive digestive enzymes in the small intestine.
- Pancreatic enzymes are active in the digestion of sugars, proteins, and fats.
- Pancreatic amylase digesting starch
- Pancreatic lipase digesting fat
- Pancreatic trypsin digesting proteins
- Pancreatic nuclease digesting nucleic acids
Pancreas also perform endocrine functions releasing hormones into the blood.
Table 1. Functions of the Digestive Organs (summary) |
||
|---|---|---|
| Organ | Major functions | Other functions |
| Mouth |
|
|
| Pharynx |
|
|
| Esophagus |
|
|
| Stomach |
|
|
| Small intestine |
|
|
| Accessory organs |
|
|
| Large intestine |
|
|
| Rectum |
|
|
| Anus |
|
|
Candela Citations
- Anatomy & Physiology. Provided by: OpenStax CNX. Located at: http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.25. License: CC BY: Attribution. License Terms: Download for free at http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.25
- Biology.. Authored by: OpenStax. Provided by: OpenStax College.. Located at: http://cnx.org/contents/185cbf87-c72e-48f5-b51e-f14f21b5eabd@9.44:1/Biology.. License: CC BY: Attribution