Pregnancy begins with the fertilization of an egg and continues through to the birth of the individual. The length of time of gestation varies among animals, but is very similar among the great apes: human gestation is 266 days, while chimpanzee gestation is 237 days, a gorilla’s is 257 days, and orangutan gestation is 260 days long. The fox has a 57-day gestation. Dogs and cats have similar gestations averaging 60 days. The longest gestation for a land mammal is an African elephant at 640 days. The longest gestations among marine mammals are the beluga and sperm whales at 460 days.
Human Gestation
Twenty-four hours before fertilization, the egg has finished meiosis and becomes a mature oocyte. When fertilized (at conception) the egg becomes known as a zygote. The zygote travels through the oviduct to the uterus ((Figure)). The developing embryo must implant into the wall of the uterus within seven days, or it will deteriorate and die. The outer layers of the zygote (blastocyst) grow into the endometrium by digesting the endometrial cells, and wound healing of the endometrium closes up the blastocyst into the tissue. Another layer of the blastocyst, the chorion, begins releasing a hormone called human beta chorionic gonadotropin (β-HCG) which makes its way to the corpus luteum and keeps that structure active. This ensures adequate levels of progesterone that will maintain the endometrium of the uterus for the support of the developing embryo. Pregnancy tests determine the level of β-HCG in urine or serum. If the hormone is present, the test is positive.
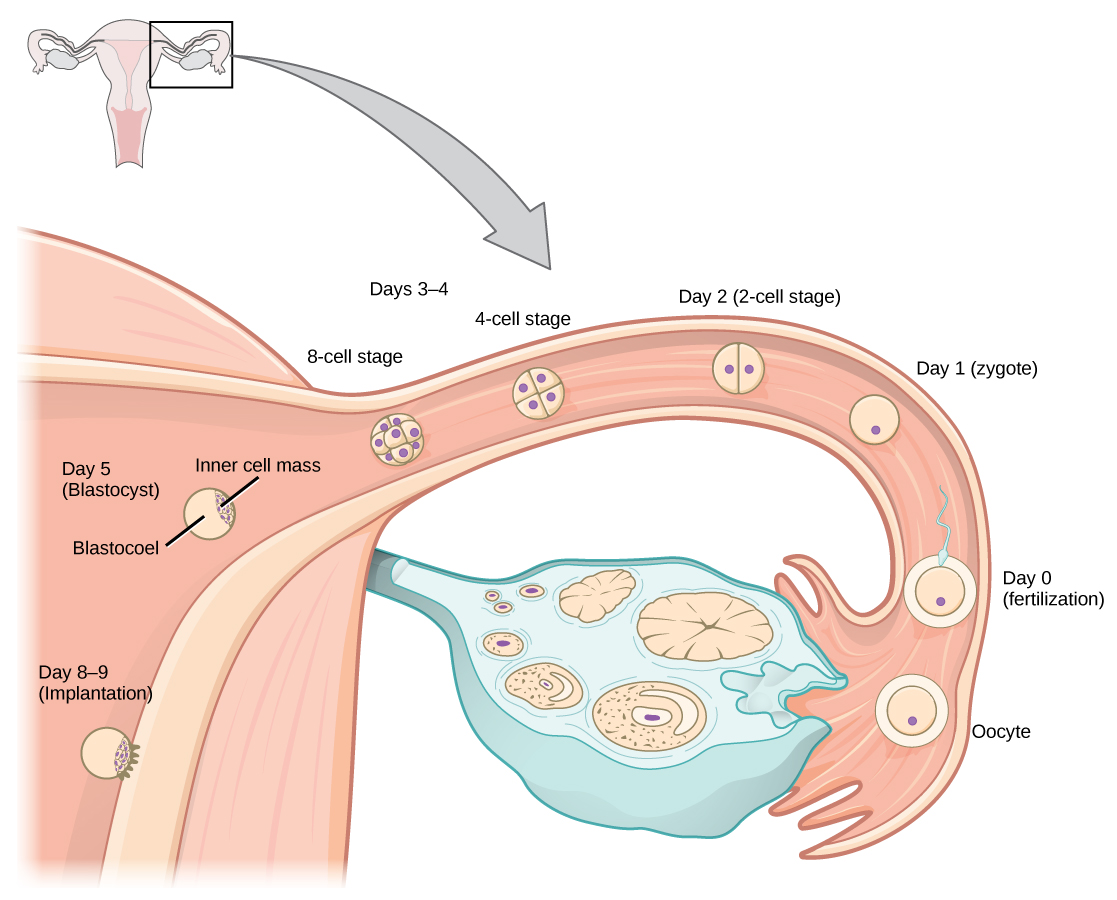
Figure 1. In humans, fertilization occurs soon after the oocyte leaves the ovary. Implantation occurs eight or nine days later.(credit: Ed Uthman)
The gestation period is divided into three equal periods or trimesters. During the first two to four weeks of the first trimester, nutrition and waste are handled by the endometrial lining through diffusion. As the trimester progresses, the outer layer of the embryo begins to merge with the endometrium, and the placenta forms. This organ takes over the nutrient and waste requirements of the embryo and fetus, with the mother’s blood passing nutrients to the placenta and removing waste from it. Chemicals from the fetus, such as bilirubin, are processed by the mother’s liver for elimination. Some of the mother’s immunoglobulins will pass through the placenta, providing passive immunity against some potential infections.
Internal organs and body structures begin to develop during the first trimester. By five weeks, limb buds, eyes, the heart, and liver have been basically formed. By eight weeks, the term fetus applies, and the body is essentially formed, as shown in (Figure). The individual is about five centimeters (two inches) in length and many of the organs, such as the lungs and liver, are not yet functioning. Exposure to any toxins is especially dangerous during the first trimester, as all of the body’s organs and structures are going through initial development. Anything that affects that development can have a severe effect on the fetus’ survival.

Figure 2. Fetal development is shown at nine weeks gestation. (credit: Ed Uthman)
During the second trimester, the fetus grows to about 30 cm (12 inches), as shown in (Figure). It becomes active and the mother usually feels the first movements. All organs and structures continue to develop. The placenta has taken over the functions of nutrition and waste and the production of estrogen and progesterone from the corpus luteum, which has degenerated. The placenta will continue functioning up through the delivery of the baby.

Figure 3. This fetus is just entering the second trimester, when the placenta takes over more of the functions performed as the baby develops. (credit: National Museum of Health and Medicine)
During the third trimester, the fetus grows to 3 to 4 kg (6 ½ -8 ½ lbs.) and about 50 cm (19-20 inches) long, as illustrated in (Figure). This is the period of the most rapid growth during the pregnancy. Organ development continues to birth (and some systems, such as the nervous system and liver, continue to develop after birth). The mother will be at her most uncomfortable during this trimester. She may urinate frequently due to pressure on the bladder from the fetus. There may also be intestinal blockage and circulatory problems, especially in her legs. Clots may form in her legs due to pressure from the fetus on returning veins as they enter the abdominal cavity.

Figure 4. There is rapid fetal growth during the third trimester. (credit: modification of work by Gray’s Anatomy)
Labor and Birth
Labor is the physical efforts of expulsion of the fetus and the placenta from the uterus during birth (parturition). Toward the end of the third trimester, estrogen causes receptors on the uterine wall to develop and bind the hormone oxytocin. At this time, the baby reorients, facing forward and down with the back or crown of the head engaging the cervix (uterine opening). This causes the cervix to stretch and nerve impulses are sent to the hypothalamus, which signals for the release of oxytocin from the posterior pituitary. The oxytocin causes the smooth muscle in the uterine wall to contract. At the same time, the placenta releases prostaglandins into the uterus, increasing the contractions. A positive feedback relay occurs between the uterus, hypothalamus, and the posterior pituitary to assure an adequate supply of oxytocin. As more smooth muscle cells are recruited, the contractions increase in intensity and force.
There are three stages to labor. During stage one, the cervix thins and dilates. This is necessary for the baby and placenta to be expelled during birth. The cervix will eventually dilate to about 10 cm. During stage two, the baby is expelled from the uterus. The uterus contracts and the mother pushes as she compresses her abdominal muscles to aid the delivery. The last stage is the passage of the placenta after the baby has been born and the organ has completely disengaged from the uterine wall. If labor should stop before stage two is reached, synthetic oxytocin, known as Pitocin, can be administered to restart and maintain labor.
An alternative to labor and delivery is the surgical delivery of the baby through a procedure called a Caesarian section. This is major abdominal surgery and can lead to post-surgical complications for the mother, but in some cases it may be the only way to safely deliver the baby.
The mother’s mammary glands go through changes during the third trimester to prepare for lactation and breastfeeding. When the baby begins suckling at the breast, signals are sent to the hypothalamus causing the release of prolactin from the anterior pituitary. Prolactin causes the mammary glands to produce milk. Oxytocin is also released, promoting the release of the milk. The milk contains nutrients for the baby’s development and growth as well as immunoglobulins to protect the child from bacterial and viral infections.
Infertility
Infertility is the inability to conceive a child or carry a child to birth. About 75 percent of causes of infertility can be identified; these include diseases, such as sexually transmitted diseases that can cause scarring of the reproductive tubes in either men or women, or developmental problems frequently related to abnormal hormone levels in one of the individuals. Inadequate nutrition, especially starvation, can delay menstruation. Stress can also lead to infertility. Short-term stress can affect hormone levels, while long-term stress can delay puberty and cause less frequent menstrual cycles. Other factors that affect fertility include toxins (such as cadmium), tobacco smoking, marijuana use, gonadal injuries, and aging.
If infertility is identified, several assisted reproductive technologies (ART) are available to aid conception. A common type of ART is in vitro fertilization (IVF) where an egg and sperm are combined outside the body and then placed in the uterus. Eggs are obtained from the woman after extensive hormonal treatments that prepare mature eggs for fertilization and prepare the uterus for implantation of the fertilized egg. Sperm are obtained from the man and they are combined with the eggs and supported through several cell divisions to ensure viability of the zygotes. When the embryos have reached the eight-cell stage, one or more is implanted into the woman’s uterus. If fertilization is not accomplished by simple IVF, a procedure that injects the sperm into an egg can be used. This is called intracytoplasmic sperm injection (ICSI) and is shown in (Figure). IVF procedures produce a surplus of fertilized eggs and embryos that can be frozen and stored for future use. The procedures can also result in multiple births.
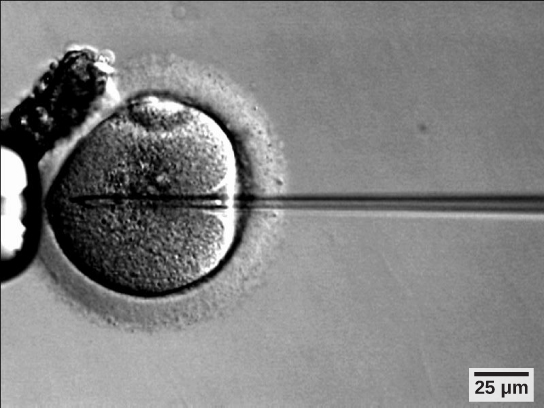
Figure 5. A sperm is inserted into an egg for fertilization during intracytoplasmic sperm injection (ICSI). (credit: scale-bar data from Matt Russell)