What is the Cardiovascular System?
The cardiovascular system, also called the circulatory system, is the organ system that transports materials to and from all the cells of the body. The materials carried by the cardiovascular system include oxygen from the lungs, nutrients from the digestive system, hormones from glands of the endocrine system, and waste materials from cells throughout the body. Transport of these and many other materials is necessary to maintain homeostasis of the body. The main components of the cardiovascular system are the heart, blood vessels, and blood. Each of these components is shown in the following figure and introduced below.

Heart
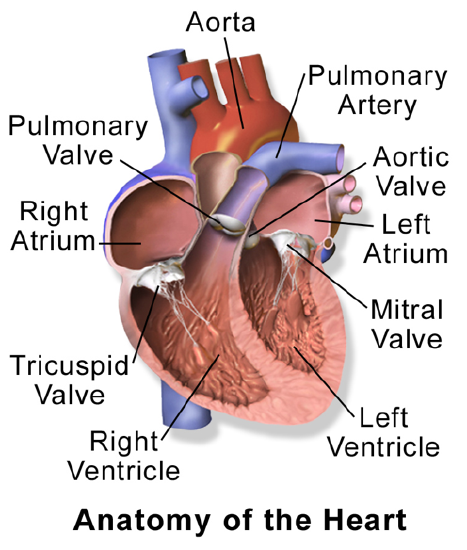
The heart is a muscular organ in the chest. It consists mainly of cardiac muscle tissue and pumps blood through blood vessels by repeated, rhythmic contractions. As shown in the figure below, the heart has four inner chambers: a right atrium and ventricle and a left atrium and ventricle. On each side of the heart, blood is pumped from the atrium to the ventricle below it and from the ventricle out of the heart. The heart also contains several valves that allow blood to flow only in the proper direction through the heart.
Unlike skeletal muscle, cardiac muscle routinely contracts without stimulation by the nervous system. Specialized cardiac muscle cells send out electrical impulses that stimulate the contractions. As a result, the atria and ventricles normally contract with just the right timing to keep blood pumping efficiently through the heart.
Blood Vessels
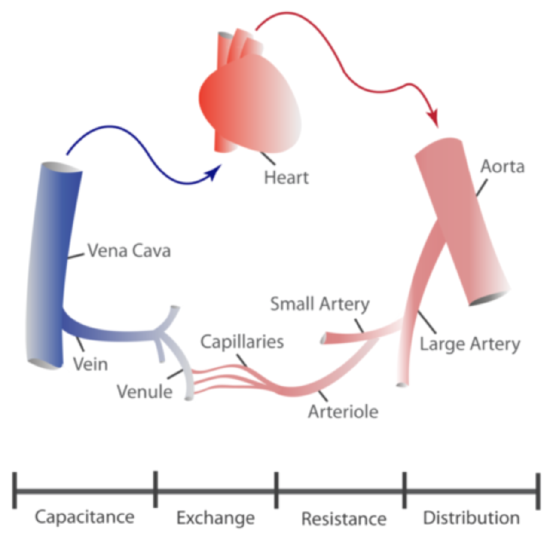
The blood vessels of the cardiovascular system are like a network of interconnected, one-way roads that range from superhighways to back alleys. Like a network of roads, the blood vessels have the job of allowing the transport of materials from one place to another. There are three major types of blood vessels: arteries, veins, and capillaries. They are illustrated in Figure 17.2.417.2.4.
- Arteries are blood vessels that carry blood away from the heart (except for the arteries that actually supply blood to the heart muscle). Most arteries carry oxygen-rich blood, and one of their main functions is distributing oxygen to tissues throughout the body. The smallest arteries are called arterioles.
- Veins are blood vessels that carry blood toward the heart. Most veins carry deoxygenated blood. The smallest veins are called venules.
- Capillaries are the smallest blood vessels. They connect arterioles and venules. As they pass through tissues, they exchange substances including oxygen with cells.
Two Circulations
Cells throughout the body need a constant supply of oxygen. They get oxygen from capillaries in the systemic circulation. The systemic circulation is just one of two interconnected circulations that make up the human cardiovascular system. The other circulation is the pulmonary system. This is where the blood picks up oxygen to carry to cells. It takes blood about 20 seconds to make one complete transit through both circulations.
Pulmonary Circulation
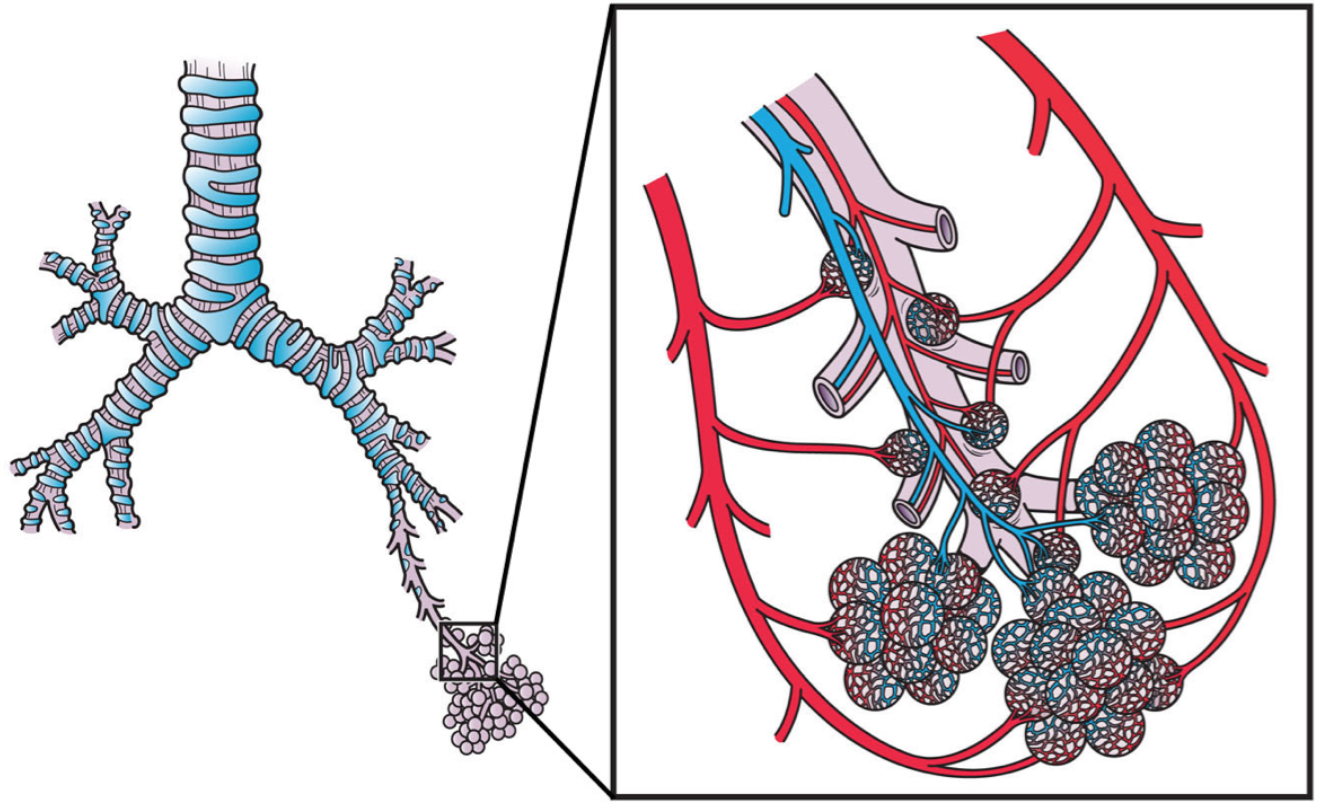
The pulmonary circulation involves only the heart and lungs and the major blood vessels that connect them. It is illustrated in the figure below. Blood moves through the pulmonary circulation from the heart to the lungs, and back to the heart again, becoming oxygenated in the process. Specifically, the right ventricle of the heart pumps deoxygenated blood into the right and left pulmonary arteries. These arteries carry the blood to the right and left lungs, respectively. Oxygenated blood then returns from the right and left lungs through the two right and two left pulmonary veins. All four pulmonary veins enter the left atrium of the heart.

What happens to the blood while it is in the lungs? It passes through increasingly smaller arteries and finally through capillary networks surrounding the alveoli (see figure below). This is where gas exchange takes place. The deoxygenated blood in the capillaries picks up oxygen from the alveoli and gives up carbon dioxide to the alveoli. As a result, the blood returning to the heart in the pulmonary veins is almost completely saturated with oxygen.
Systemic Circulation
The oxygenated blood that enters the left atrium of the heart in the pulmonary circulation then passes into the systemic circulation. This is the part of the cardiovascular system that transports blood to and from all of the tissues of the body to provide oxygen and nutrients and pick up wastes. It consists of the heart and blood vessels that supply the metabolic needs of all the cells in the body, including those of the heart and lungs.

As shown in Figure 17.2.717.2.7, in the systemic circulation, the left atrium pumps oxygenated blood to the left ventricle, which pumps the blood directly into the aorta, the body’s largest artery. Major arteries branching off the aorta carry the blood to the head and upper extremities. The aorta continues down through the abdomen and carries blood to the abdomen and lower extremities. The blood then returns to the heart through the network of increasingly larger veins of the systemic circulation. All of the returning blood eventually collects in the superior vena cava (upper body) and inferior vena cava (lower body), which empty directly into the right atrium of the heart.
Blood
Blood is a fluid connective tissue that circulates throughout the body in blood vessels by the pumping action of the heart. Blood carries oxygen and nutrients to all the body’s cells, and it carries carbon dioxide and other wastes away from the cells to be excreted. Blood also transports many other substances, defends the body against infection, repairs body tissues, and controls the body’s pH, among other functions.
The fluid part of blood is called plasma. It is a yellowish, watery liquid that contains many dissolved substances and blood cells. Types of blood cells in plasma include red blood cells, white blood cells, and platelets, all of which are illustrated in the following photomicrograph and described below.

- Red blood cells have the main function of carrying oxygen in the blood. Red blood cells consist mostly of hemoglobin, a protein containing iron that binds with oxygen.
- White blood cells are far fewer in number than red blood cells. They defend the body in various ways. For example, white blood cells called phagocytes swallow and destroy pathogens, dead cells, and other debris in the blood.
- Platelets are cell fragments involved in blood clotting. They stick to tears in blood vessels and to each other, forming a plug at the site of injury. They also release chemicals that are needed for clotting to occur.
Structure of the Heart
The heart has a thick muscular wall that consists of several layers of tissue. Internally, the heart is divided into four chambers through which blood flows. Blood flows in just one direction through the chambers due to heart valves.
Heart Wall
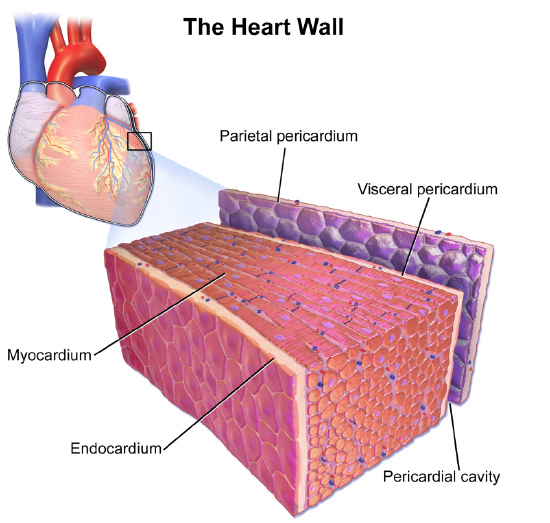
As shown in the figure below, the wall of the heart is made up of three layers, called the endocardium, myocardium, and pericardium.
- The endocardium is the innermost layer of the heart wall. It is made up primarily of simple epithelial cells. It covers the heart chambers and valves. A thin layer of connective tissue joins the endocardium to the myocardium.
- The myocardium is the middle and thickest layer of the heart wall. It consists of cardiac muscle surrounded by a framework of collagen. There are two types of cardiac muscle cells in the myocardium: pacemaker cells, which have the ability to contract easily; and pacemaker cells, which conduct electrical impulses that cause the cardiomyocytes to contract. About 99 percent of cardiac muscle cells are cardiomyocytes, and the remaining 1 percent are pacemaker cells. The myocardium is supplied with blood vessels and nerve fibers via the pericardium.
- The epicardium is the third layer which is a part of the pericardium, a protective sac that encloses and protects the heart. The pericardium consists of two membranes (visceral pericardium called epicardium and parietal pericardium), between which there is a fluid-filled cavity. The fluid helps to cushion the heart and also lubricates its outer surface.
Heart Chambers
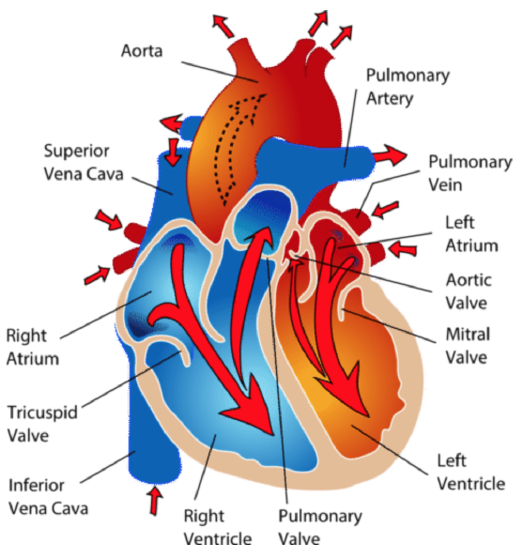
As shown in Figure 17.3.317.3.3, the four chambers of the heart include two upper chambers called atria (singular, atrium) and two lower chambers called ventricles. The atria are also referred to as receiving chambers because blood coming into the heart first enters these two chambers. The right atrium receives blood from the upper and lower body through the superior vena cava and inferior vena cava, respectively; and the left atrium receives blood from the lungs through the pulmonary veins. The ventricles are also referred to as discharging chambers because the blood leaving the heart passes out through these two chambers. The right ventricle discharges blood to the lungs through the pulmonary artery, and the left ventricle discharges blood to the rest of the body through the aorta. The four chambers are separated from each other by dense connective tissue consisting mainly of collagen.
Heart Valves
The diagram above also shows the location of the four valves of the heart. The heart valves allow blood to flow from the atria to the ventricles and from the ventricles to the pulmonary artery and aorta. The valves are constructed in such a way that blood can flow through them in only one direction, thus preventing the backflow of blood. The four valves are the:
- tricuspid valve, which allows blood to flow from the right atrium to the right ventricle.
- the mitral valve, which allows blood to flow from the left atrium to the left ventricle.
- pulmonary valve, which allows blood to flow from the right ventricle to the pulmonary artery.
- the aortic valve, which allows blood to flow from the left ventricle to the aorta.
The tricuspid and mitral valves are also called atrioventricular (or AV) valves because they are found between the atrium and the ventricle. The pulmonary and aortic valves are also called semilunar valves because they are shaped like half-moons.
Coronary Circulation
The cardiomyocytes of the muscular walls of the heart are very active cells because they are responsible for the constant beating of the heart. These cells need a continuous supply of oxygen and nutrients. The carbon dioxide and waste products they produce also must be continuously removed. The blood vessels that carry blood to and from the heart muscle cells make up the coronary circulation. Note that the blood vessels of the coronary circulation supply heart tissues with blood and are different from the blood vessels that carry blood to and from the chambers of the heart as part of the general circulation. Coronary arteries supply oxygen-rich blood to the heart muscle cells. Coronary veins remove deoxygenated blood from the heart muscle cells.
- There are two coronary arteries: a right coronary artery that supplies the right side of the heart and a left coronary artery that supplies the left side of the heart. These arteries branch repeatedly into smaller and smaller arteries and finally into capillaries, which exchange gases, nutrients, and waste products with cardiomyocytes.
- At the back of the heart, small cardiac veins drain into larger veins and finally into the great cardiac vein, which empties into the right atrium. At the front of the heart, small cardiac veins drain directly into the right atrium.
Blood Circulation Through the Heart
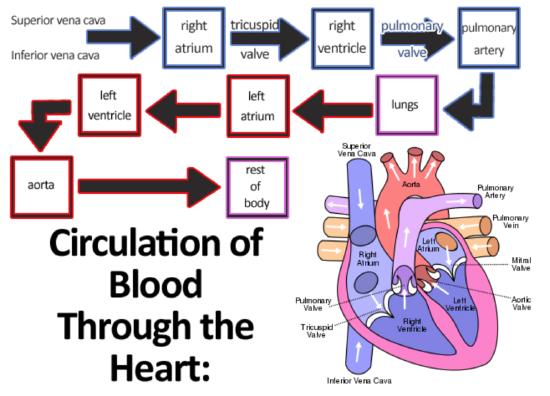
The diagram below shows how blood circulates through the chambers of the heart. The right atrium collects blood from two large veins, the superior vena cava (from the upper body) and the inferior vena cava (from the lower body). The blood that collects in the right atrium is pumped through the tricuspid valve into the right ventricle. From the right ventricle, the blood is pumped through the pulmonary valve into the pulmonary artery. The pulmonary artery carries the blood to the lungs, where it enters the pulmonary circulation, gives up carbon dioxide, and picks up oxygen. The oxygenated blood travels back from the lungs through the pulmonary veins (of which there are four) and enters the left atrium of the heart. From the left atrium, the blood is pumped through the mitral valve into the left ventricle. From the left ventricle, the blood is pumped through the aortic valve into the aorta, which subsequently branches into smaller arteries that carry the blood throughout the rest of the body. After passing through capillaries and exchanging substances with cells, the blood returns to the right atrium via the superior vena cava and inferior vena cava, and the process begins anew.
Cardiac Cycle
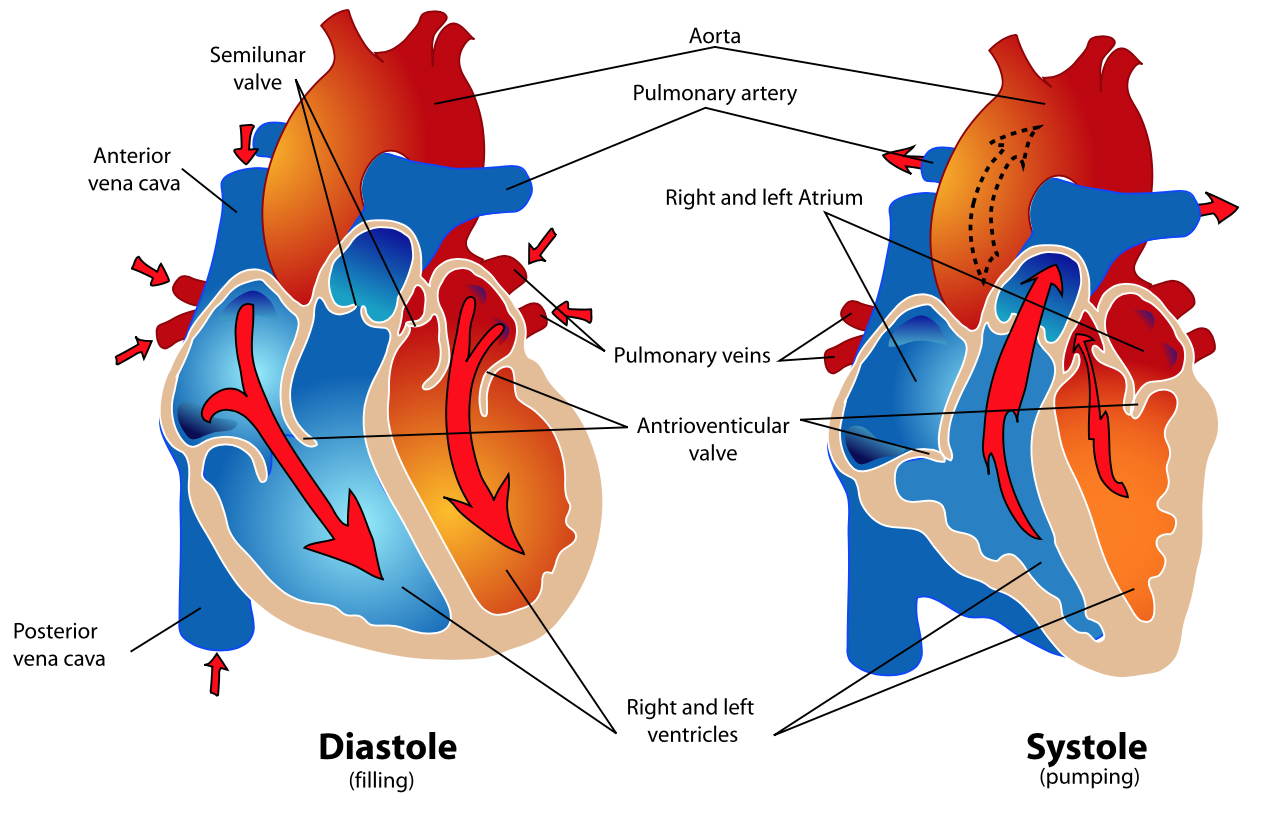
The cardiac cycle refers to a single complete heartbeat, which includes one iteration of the lub and dub sounds heard through a stethoscope. During the cardiac cycle, the atria and ventricles work in a coordinated fashion so that blood is pumped efficiently through and out of the heart. The cardiac cycle includes two parts, called diastole and systole, which are illustrated in Figure 17.3.517.3.5.
- During diastole, the atria contract and pump blood into the ventricles, while the ventricles relax and fill with blood from the atria.
- During systole, the atria relax and collect blood from the lungs and body, while the ventricles contract and pump blood out of the heart.
Electrical Stimulation of the Heart
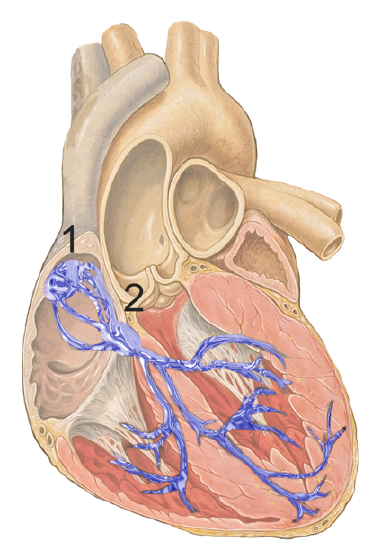
The normal, rhythmical beating of the heart is called sinus rhythm. It is established by the heart’s pacemaker cells, which are located in an area of the heart called the sinoatrial node (shown in the figure below). The pacemaker cells create electrical signals by the movement of electrolytes (sodium, potassium, and calcium ions) into and out of the cells. For each cardiac cycle, an electrical signal rapidly travels first from the sinoatrial node to the right and left atria so they contract together. Then the signal travels to another node, called the atrioventricular node (also shown below), and from there to the right and left ventricles, which also contract together, just a split second after the atria contract.
The normal sinus rhythm of the heart is influenced by the autonomic nervous system through sympathetic and parasympathetic nerves. These nerves arise from two paired cardiovascular centers in the medulla of the brainstem. The parasympathetic nerves act to decrease the heart rate, and the sympathetic nerves act to increase the heart rate. Parasympathetic input normally predominates. Without it, the pacemaker cells of the heart would generate a resting heart rate of about 100 beats per minute, instead of a normal resting heart rate of about 72 beats per minute. The cardiovascular centers receive input from receptors throughout the body and act through the sympathetic nerves to increase the heart rate as needed. For example, increased physical activity is detected by receptors in muscles, joints, and tendons. These receptors send nerve impulses to the cardiovascular centers, causing sympathetic nerves to increase the heart rate. This allows more blood to flow to the muscles.
Besides the autonomic nervous system, other factors can also affect the heart rate. For example, thyroid hormones and adrenal hormones such as epinephrine can stimulate the heart to beat faster. The heart rate also increases when blood pressure drops or the body is dehydrated or overheated. On the other hand, cooling of the body and relaxation, among other factors, can contribute to a decrease in the heart rate.
What Is Cardiovascular Disease?
Cardiovascular disease is a class of diseases that involve the cardiovascular system. They include diseases of the coronary arteries that supply the heart muscle with oxygen and nutrients; diseases of arteries such as the carotid artery that provide blood flow to the brain; and diseases of the peripheral arteries that carry blood throughout the body. Worldwide, cardiovascular disease is the leading cause of death, causing about a third of all deaths each year.
Most cases of cardiovascular disease occur in people over the age of 60, with disease onset typically being about a decade earlier in males than females. The LGBT (lesbian, gay, bisexual, and transgender) community belongs to almost every race, ethnicity, religion, age, and socioeconomic group. The LGBT youth are at a higher risk for cardiovascular diseases, obesity, anxiety, and depression as compared to the general population. LGBT youth receive poor quality of care due to stigma, lack of healthcare providers’ awareness, and insensitivity to the unique needs of this community. Young LGBT individuals find it difficult to report their sexual identity to their clinicians. Some clinicians are not well trained in addressing the concerns of members of this community.
You can’t control your age or sex, but you can control other factors that increase the risk of cardiovascular disease. Not smoking, maintaining a healthy weight, eating a healthy diet, taking medications as needed to control diabetes and cholesterol, and getting regular exercise are all ways to prevent cardiovascular disease or keep it from progressing. It should be noted that high blood lipid levels are definitely risk factors for cardiovascular disease. High levels of cholesterol in the diet do not appear to lead directly to high levels of cholesterol in the blood. Clearly, cardiovascular disease is multifactorial in terms of its causes.
Precursors of Cardiovascular Disease
There are two very common conditions that are precursors to virtually all cases of cardiovascular disease: hypertension (hypertension) and atherosclerosis (hardening of blood wall). Both conditions affect the arteries and their ability to maintain normal blood flow.
Hypertension
Hypertension is a chronic medical condition in which the blood pressure in the arteries is persistently elevated, as defined in the table below. Hypertension usually does not cause symptoms, so more than half of the people with high blood pressure are unaware of their condition. Hypertension is typically diagnosed when blood pressure is routinely measured during a medical visit for some other health problem.
|
Category |
Systolic (mm Hg) |
Diastolic (mm Hg) |
|---|---|---|
|
Normal blood pressure |
90-119 |
60-79 |
|
Prehypertension |
120-139 |
80-89 |
|
Hypertension |
140 or higher |
90 or higher |
High blood pressure is classified as either primary or secondary high blood pressure. At least 90% of cases are primary high blood pressure, which is caused by some combination of genetic and lifestyle factors. Numerous genes have been identified as having small effects on blood pressure. Lifestyle factors that increase the risk of high blood pressure include excess dietary salt and alcohol consumption in addition to the risk factors for cardiovascular disease stated above. Secondary high blood pressure, which makes up the remaining 10% of cases of hypertension, is attributable to chronic kidney disease or an endocrine disorder such as Cushing’s disease.
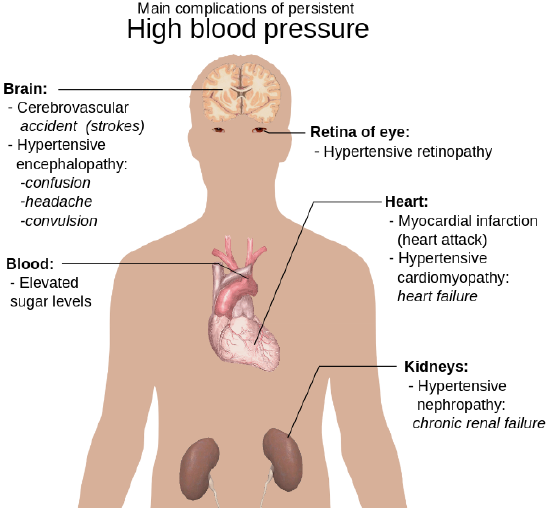
Treating hypertension is important for reducing the risk of all types of cardiovascular disease, especially stroke. These and other complications of persistent high blood pressure are shown in the figure below. Lifestyle changes, such as reducing salt intake and adopting a healthier diet (such as the DASH diet outlined in the Feature below) may be all that is needed to lower blood pressure to the normal range. In many cases, however, medications are also required.
Atherosclerosis
Atherosclerosis is a condition in which artery walls thicken and stiffen as a result of the buildup of plaques inside the arteries. Plaques consist of white blood cells, cholesterol, and other fats. Typically, there is also a proliferation of smooth muscle cells that make the plaque fibrous as well as fatty. Over time, the plaques may harden with the addition of calcium crystals. This reduces the elasticity of the artery walls. As plaques increase in size, the artery walls dilate to compensate so blood flow is not affected. Eventually, however, the lumen of the arteries is likely to become so narrowed by plaque buildup that blood flow is reduced or even blocked entirely. The figure below illustrates the formation of a plaque in a coronary artery.
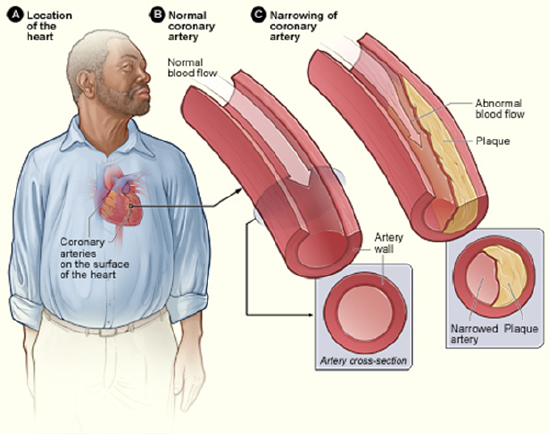
In most people, plaques start to form in arteries during childhood and progress throughout life. Individuals may develop just a few plaques or dozens of them. Plaques typically remain asymptomatic for decades. Signs and symptoms appear only after there is severe narrowing (stenosis) or complete blockage of arteries. As plaques increase in size and interfere with blood flow, they commonly lead to the formation of blood clots. These may plug arteries at the site of the plaque or travel elsewhere in the circulation. Sometimes plaques rupture or become detached from an arterial wall and become lodged in a smaller, downstream artery. Blockage of arteries by plaques or clots may cause a heart attack, stroke, or other potentially life-threatening cardiovascular events. If blood flow to the kidneys is affected, it may lead to chronic kidney disease.
The process in which plaques form is not yet fully understood, but it is thought that it begins when low-density lipoproteins (LDLs) accumulate inside endothelial cells in artery walls, causing inflammation. The inflammation attracts white blood cells that start to form a plaque. Continued inflammation and a cascade of other immune responses cause the plaque to keep growing. Risk factors for the development of atherosclerosis include hypertension, high cholesterol (especially LDL cholesterol), diabetes, and smoking. The chance of developing atherosclerosis also increases with age, male sex, and a family history of cardiovascular disease.
Treatment of atherosclerosis often includes both lifestyle changes and medications to lower cholesterol, control blood pressure, and reduce the risk of blood clot formation. In extreme cases or when other treatments are inadequate, surgery may be recommended. Surgery may involve the placement of stents in arteries to keep them open and improve blood flow or the use of grafts to divert blood flow around blocked arteries.
Coronary Artery Disease
Coronary artery disease is a group of diseases that result from atherosclerosis of coronary arteries. Treatment of the diseases mainly involves treating underlying atherosclerosis. Two of the most common coronary artery diseases are angina and myocardial infarction.
Angina
Angina is chest pain or pressure that occurs when heart muscle cells do not receive adequate blood flow and become starved of oxygen (a condition called ischemia). It is illustrated in Figure 17.7.417.7.4. There may also be pain in the back, neck, shoulders, or jaw; and in some cases, the pain may be accompanied by shortness of breath, sweating, or nausea. The main goals of the treatment of angina are relieving the symptoms and slowing the progression of underlying atherosclerosis.
Angina may be classified as either stable angina or unstable angina:
- Stable angina is angina in which pain is precipitated by exertion (say, from brisk walking or running) and improves quickly with rest or the administration of nitroglycerin, which dilates coronary arteries and improves blood flow. Stable angina may develop into unstable angina.
- Unstable angina is angina in which pain occurs during rest, lasts more than 15 minutes, and is of new onset. This type of angina is more dangerous and may be a sign of an imminent heart attack. It requires urgent medical attention.
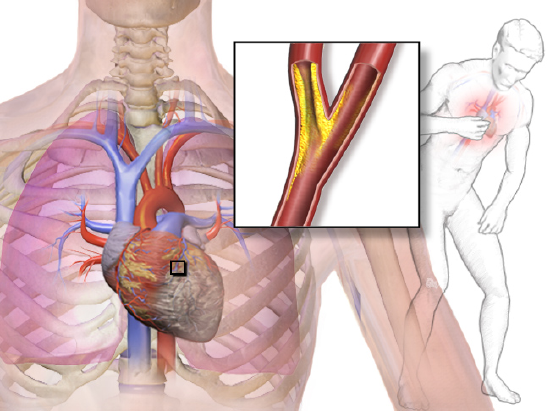
Myocardial Infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow stops to a part of the heart causing damage to the heart muscle and the death of myocardial cells. As shown in the figure below, an MI usually occurs because of complete blockage of a coronary artery, often due to a blood clot or the rupture of a plaque (see figure below). An MI typically causes chest pain and pressure, among other possible symptoms, but at least one-quarter of MIs do not cause any symptoms.
In the worst case, an MI may cause sudden death. Even if the patient survives, an MI often causes permanent damage to the heart. This puts the heart at risk of heart arrhythmias, heart failure, and cardiac arrest.
- Heart arrhythmias are abnormal heart rhythms, which are potentially life-threatening. Heart arrhythmias often can be interrupted with a cardiac defibrillator, which delivers an electrical shock to the heart, in effect “rebooting” it.
- Heart failure occurs when the pumping action of the heart is impaired so tissues do not get adequate oxygen. This is a chronic condition that tends to get worse over time, although it can be managed with medications.
- Cardiac arrest occurs when the heart no longer pumps blood or pumps blood so poorly that vital organs can no longer function. This is a medical emergency requiring immediate intervention.
Other Cardiovascular Diseases
Hypertension and atherosclerosis often cause other cardiovascular diseases. These commonly include stroke and peripheral artery disease.
Stroke
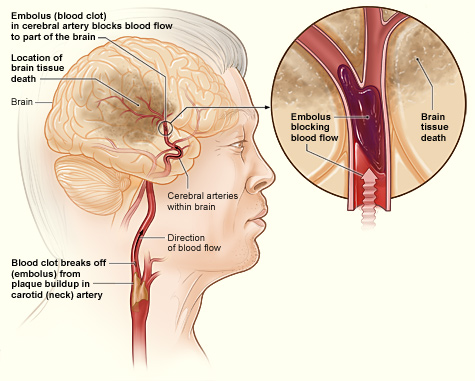
A stroke, also known as a cerebrovascular accident or brain attack, occurs when blocked or broken arteries in the brain result in the death of brain cells. There are two main types of stroke, both of which are illustrated below: ischemic stroke and hemorrhagic stroke.
- An ischemic stroke occurs when an embolus (blood clot) breaks off from a plaque or forms in the heart because of arrhythmia and travels to the brain where it becomes lodged in an artery. This blocks blood flow to the part of the brain that is served by arteries downstream from the blockage. Lack of oxygen causes the death of brain cells. Treatment with a clot-busting drug within a few hours of the stroke may prevent permanent damage. Almost 90 percent of strokes are ischemic strokes.
- A hemorrhagic stroke occurs when an artery in the brain ruptures and causes bleeding in the brain. This deprives downstream tissues of adequate blood flow and also puts pressure on brain tissue. Both factors can lead to the death of brain cells. Surgery to temporarily open the cranium may be required to relieve the pressure. Only about 10 percent of strokes are hemorrhagic strokes, but they are more likely to be fatal than ischemic strokes.
In both types of stroke, the part of the brain that is damaged loses is the ability to function normally. Signs and symptoms of stroke may include an inability to move, feel, or see on one side of the body; problems understanding speech or difficulty speaking; memory problems; confusion; and dizziness. Hemorrhagic strokes may also cause a severe headache. The symptoms of a stroke usually occur within seconds or minutes of the brain injury. Depending on the severity of the stroke and how quickly treatment is provided, the symptoms may be temporary or permanent. If the symptoms of a stroke go away on their own in less than an hour or two, the stroke is called a transient ischemic attack. Stroke is the leading cause of disability in the United States, but rehabilitation with physical, occupational, speech, or other types of therapy may significantly improve functioning.
The main risk factor for stroke is high blood pressure. Therefore, keeping blood pressure within the normal range, whether with lifestyle changes or medications, is the best way to reduce the risk of stroke. Another possible cause of stroke is the use of illicit drugs such as amphetamines or cocaine. Having had a stroke in the past greatly increases one’s risk of future strokes. Men are also more likely than women to have strokes.
Peripheral Artery Disease
Peripheral artery disease (PAD) is the narrowing of the arteries other than those that supply the heart or brain due to atherosclerosis. The figure below shows how the PAD occurs. PAD most commonly affects the legs, but other arteries may also be involved. The classic symptom is leg pain when walking, which usually resolves with rest. This symptom is known as intermittent claudication. Other symptoms may include skin ulcers, bluish skin, cold skin, or poor nail and hair growth in the affected leg(s). However, up to half of all cases of PAD do not have any symptoms.
The main risk factor for PAD is smoking. Other risk factors include diabetes, high blood pressure, and high blood cholesterol. The underlying mechanism is usually atherosclerosis. PAD is typically diagnosed when blood pressure readings taken at the ankle are lower than blood pressure readings taken at the upper arm. It is important to diagnose PAD and treat underlying atherosclerosis because people with this disorder have a four to five times higher risk of myocardial infarction or stroke. Surgery to expand the affected arteries or to graft vessels in order to bypass blockages may be recommended in some cases.
Feature: My Human Body
You read in this concept about the many dangers of hypertension. Do you know whether you have hypertension? The only way to know for sure is to have your blood pressure measured. Measuring blood pressure is quick and painless, but several measurements are needed to accurately diagnose hypertension. Some people have what is called “white coat disease.” Their blood pressure rises just because they are being examined by a physician (in a white coat). Blood pressure also fluctuates from time to time due to factors such as hydration, stress, and time of day. Repeatedly measuring and recording your own blood pressure at home can provide your doctor with valuable diagnostic data. Digital blood pressure monitors for home use, like the one pictured below, are relatively inexpensive, easy to use, and available at most pharmacies.

Candela Citations
- Cardiovascular System. Authored by: Contributed by Suzanne Wakim & Mandeep Grewal Professors (Cell Molecular Biology & Plant Science) at Butte College. Located at: https://bio.libretexts.org/Bookshelves/Human_Biology/Book%3A_Human_Biology_(Wakim_and_Grewal)/17%3A_Cardiovascular_System/17.2%3A_Introduction_to_the_Cardiovascular_System. Project: Book: Human Biology (Wakim & Grewal). License: CC BY-NC: Attribution-NonCommercial
