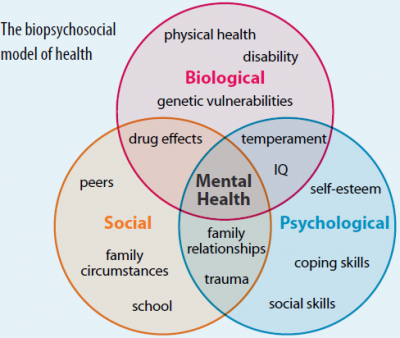
Cognitive Behavioral Therapy (CBT) is a method that can help manage problems by changing the way patients would think and behave. It is not designed to remove any problems but help manage them in a positive manner [14] [15]. According to Monticone et al., (2013), CBT is classified as a psychological management to be used in the case of chronic pain. This is usually done in conjunction with other physical modalities and exercise forms.[16] The purpose of CBT is to incorporate behavioral and cognitive elements that occurs in the pain experience by the patient.[17] This therapy concerns for the individuals’ social functioning, quality of life and overall physical function. [17] It utilize many principles to assist the patient to redefine the concept of pain, and allow room to shift the perception of negative and threatening thoughts into something understandable. Therapists will work from this established personal aims and goals to lay out possible realistic treatments plan to assist the patient in achieving their goals and overcoming the cognitive and behavioral problems that they may experience in the process.[18]
CBT is created to make changes to how an individual think, it challenge pain related beliefs and therefore influencing the patient’s perception. The therapy process is broken down into parts (for example: behavioral changes implementations and cognitive reconditioning). [17]
The Six Phases of CBT
There are six phases involved in CBT: 1. Assessment (assess patient’s information through self-reported questions and observations), 2.Reconceptualisation (patient will require to keep a self-report diary with the intention to assist patients with questions regarding to negative and/or manipulative thoughts) , 3. Skills acquisition and consolidation (the therapist will use cognitive and behavioral techniques to educate patient to deal with challenged that affect their day to day lives, this may include, problem solving and relaxation skills), 4. Skills consolidation and application (where patients are given tasks to assist them to reinforce the skills they have been taught to handle their thoughts), 5. Generalization and maintenance (where review of patient’s tasks and skill practice will be given, they will be given evaluation of their progress in order to successfully enhance their coping skills) and 6. Post-treatment and follow up (the therapist will review the patients progression in entirety and how well the patient can apply the CBT in their day to day living activities).[19]
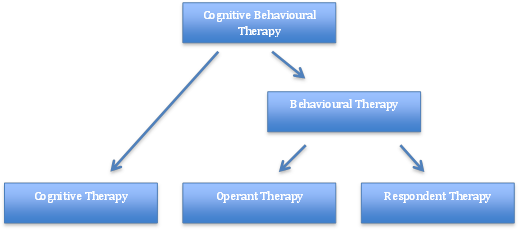
Behavior therapy (BT) was developed in the 1950’s independently in three countries: South Africa, USA and England [20]. It was further developed to Cognitive Therapy (CT) in the 1970’s by Dr Aaron Beck with its main application on people with depression, anxiety and eating disorders [14] [21]. However, the main evidence today focuses on CBT, after the merging of BT and CT in the late 80’s [22].
Fig.2 – Breakdown of CBT theory
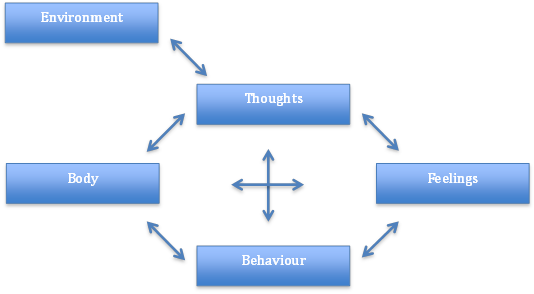
Fig.3 – Factors involved within the Cognitive Behavioral Therapy Model
Aaron Beck and Christine Padesky first recognized this CBT model in the 1970s [23].
How it is used:
- Negative thoughts (e.g., “My back pain is uncontrollable” –> Negative feelings (e.g., depression, anger) and maladaptive health behaviors (e.g., skipping treatment sessions) –> Reinforcing negative cycle.
If one negative thought can be changed or better understood, then it can break down this negative cycle. This can be addressed through education and methods to manage symptoms [23].
There are 3 basic principles of CBT [27]:
- How people think about their situations, influences how they feel and what they do.
- Problems like depression, anxiety and self-defeating behavior can be broken down by problematic thought patterns.
- People can learn to identify distorted thinking, change their outlook, take constructive action, and feel better.
Advantages and Disadvantages
| Advantages |
Disadvantages |
| The highly structured nature of CBT means it can be provided in different formats, including in groups, self-help books and computer programs. | Does not use a holistic approach to a patient’s situation. |
| Skills learnt through CBT are useful, practical and helpful. These strategies can be incorporated into daily lifestyle and benefit the management with future stresses and difficulties. | Due to the structured nature of CBT, it may not be suitable for people with more complex mental health needs or learning difficulties. |
| CBT can be sustained long term | Commitment is required from the patient. A therapist can help and advise them, but may be unsuccessful without co-operation from the patient. |
Outcome Measures
Outcome Measures for CBT are varied regarding their intended use. Certain outcome measures will be used for:
- Pain
- Disability
- Depression/Anxiety
- Patient Thought’s and Beliefs
Examples of Outcome Measures are shown below:
- Roland Morris Disability Questionnaire
- Pain Anxiety Symptom Scale (PASS) – The Pain Anxiety Symptom Scale (PASS) is used as a measure to evaluate the patients ‘fear of pain’. It is intended to provide a means of ‘fear of pain’ in exaggerated or persistent pain behaviors [28]. This was created because anxious responses can lead to avoidance behaviors that can then lead to chronic pain. The Pain Anxiety Symptom Scale has been classed as having a high level of validity when used in clinical practice [29].
- Chronic Pain Acceptance Questionnaire – The Chronic Pain Acceptance Questionnaire is a 20-Item Scale that covers two components; Activity Engagement and Pain Willingness. Activity Engagement is used in accordance to measure patient’s participation in activities regardless of pain, while Pain Willingness assesses relative absence of attempts to control or avoid pain[30]. This outcome measure has been found to have a good scale of reliability [31].
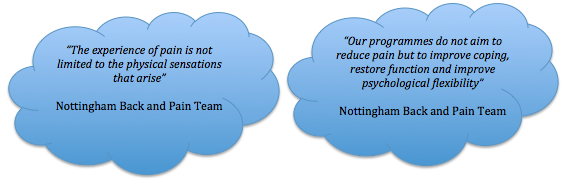
Fig. 5 Quotes from experienced clinicians
Cognitive Therapy (CT)
Cognitive Therapy was developed and pioneered by Dr Aaron Beck in the 1960’s. During this time, it was employed as an information-processing model to understand and treat psychopathological conditions.
Cognitive Therapy – The Theory
Cognitive Therapy (CT), as mentioned above, is one part of the entire CBT model and an approach to treating chronic pain. This process proposes that distorted or dysfunctional thinking can influence a patient’s mood and psychological beliefs, which has been found to coincide with chronic pain [14] [32] [33].
This treatment involves the identification and replacement of misrepresented thoughts and beliefs that a patient could be feeling. Cognitive Therapy is a problem-solving treatment based on the principle that we perceive situations, influences how we feel about them [34].
The effectiveness of CT has shown positive outcomes regarding depression and anxiety disorders. Alongside these psychological benefits, it has provided positive results concerning certain medical issues, including chronic fatigue syndrome and other chronic pain disorders [35].
- Fig.6 Concept of Cognitive Therapy
Principles of CT
There are 5 principles of CT that patients learn throughout each individual session:
- Distinguishing between thoughts and feelings
- Becoming aware of the ways that thoughts can influence feelings, that can be detrimental and harmful.
- Learning about thoughts that seem to occur automatically, without even realizing how they may affect emotions.
- Critical evaluation of whether these automatic assumptions are accurate.
- Developing skills to notice, interrupt, and correct these thoughts independently [36].
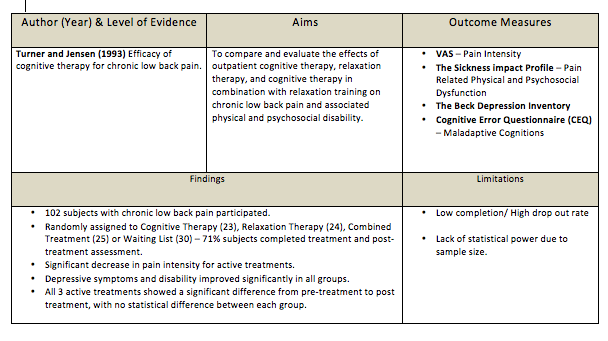
CT on Chronic Low Back Pain- The Evidence
Limited evidence of Cognitive Therapy on the effect of Chronic Low Back Pain is available [37]. The following table is a breakdown of a randomized controlled trial on CT for Chronic Low Back Pain.
Behavioral Therapy (BT)
Behavioral Therapy (BT) was developed in the 1950’s. It was originally used to treat psychological issues such as depression but has been used more recently to treat other conditions such as CLBP.
Behavioral Therapy is split into two areas – Operant Therapy and Respondent Therapy. Both parts of Behavioural Therapy look at changing detrimental behaviors to more healthy and positive behaviors [38].
Operant Therapy (OT)
Operant therapy is based on the Operant Conditioning principles, first proposed by Skinner (1953) in his book, Science and Human Behavior. The Operant behavioral model was first applied to CLBP by Fordyce (1976), in his book Behavioral Methods for Chronic pain and Illness [39].
OT – The Theory
Operant Behavioral Therapy or Operant Conditioning proposes that pain behaviors learnt by an individual can be reinforced by external factors [39] [40]. These external factors are positive reinforcements of the pain behaviors, used by the patient, which can be detrimental to their long term health. These factors often include detrimental attention from family, medical personnel, dependency on pain medication and excessive rest. Therefore, operant behavioral therapy looks at removing these damaging, positive reinforcements, and replacing them with more healthy behavior. Operant behavioral techniques often involve the use of increased exercise levels, and work to meet targets set by the patient and clinician. This method can also be helped by incorporating the family and friends of the patient, to maintain and monitor the change back to more healthy behaviors. With each goal that is achieved, the patient is positively reinforced by all staff and personnel involved [39].
Uses in Clinical Practice
Operant Therapy is used in a variety of clinical settings [40]. Operant therapy is primarily used to treat psychological issues, such as depression and anxiety. It has also been used as part of a Multi-disciplinary approach to treating long term conditions, such as CLBP and Fibromyalgia [42]; [39]. Thieme et al. (2007) looked at the effects of Operant Behaviour therapy on 125 Fibromyalgia patients. After a 12 month follow up, it showed that 53.5% of patients in the Operant Therapy group had meaningful improvements in pain intensity.
Respondent Therapy (RT) – The Theory
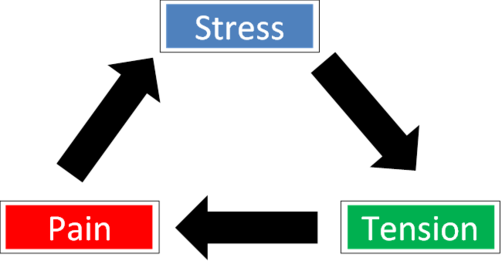
Respondent therapy is an approach to behavioral therapy with aims to modify the body’s physiological response to pain, by reducing muscular tension [39]. The respondent model, as described by Gentry and Bernal (1977) [43], theorizes that physical damage can lead to a pain-tension cycle.
Fig. 7 Diagram to represent the Pain-Tension Cycle in a simplified manner.
Pain-Tension Cycle
This cycle is viewed as a cause and a result of muscular tension [44]. It states that whilst avoidance of movement may be used to reduce pain, the resulting decreased mobility may increase the tension, and thus pain furthermore. Respondent therapy aims to disrupt this cycle using methods such as relaxation, progressive relaxation, applied relaxation and Electromyographic (EMG) feedback. These methods are used to reduce the muscular tension, relieving anxiety and thus the subsequent pain [44] [45].
Techniques for RT
Progressive relaxation is a technique for learning to monitor and control the state of muscular tension [46]. It was developed by American physician Edmund Jacobson in the early 1920s. The technique involves learning to monitor tension in each specific muscle group in the body by deliberately inducing tension in each group. Upon releasing this tension, attention is paid to the contrast between tension and relaxation. It is to be noted that these are not considered to be exercises or hypnotism.
The “Applied Relaxation” protocol developed in Sweden, by the psychologist Lars-Goran Öst, modified from Jacobson’s progressive relaxation technique. It expands on progressive relaxation but involves attempting to relax more quickly and in different scenarios [47].
EMG feedback, in respondent therapy, is used as a point of reference for a patient to objectify their muscle relaxation techniques [48]. It uses several surface electrodes to detect the action potentials of muscles, giving appropriate feedback as to the state of muscular contraction.
Evidence for RT
Several studies have compared respondent therapy using progressive relaxation to a placebo [49] [50] [37]. Results showed favorable effects of the active treatment, which was not statistically significant, as the waiting list control also showed improvements.
Four studies have identified respondent therapy with EMG feedback against a placebo[51]; [52]; [48]; [49]). These studies showed slightly favorable results for the intervention but produced no significant results.
Evidence of Effectiveness Against Other Forms of Therapy
One study compared respondent therapy against self-hypnosis [53]. It concluded that neither intervention were superior to the other due its non-significant results compared to the placebo.
Evidence of Effectiveness of Respondent Therapy in Addition To Other Treatments
One study compared a combination of respondent therapy with EMG feedback, and physiotherapy, with physiotherapy alone [54]. Significant differences noted in favor of the combined intervention for pain post-treatment, after 6 weeks and 6 months.
Cognitive vs Behavioral Therapy on CLBP – The Evidence
A study [55] compared cognitive and operant therapy. Both groups also received physiotherapy in the form of an exercise program and education, for the management of back pain. The operant therapy group reported a significant improvement in general function status but did not find the same results for pain intensity. The quality of this study is in question, as a systematic review by Middlekoop et al,. (2011) [56] reported that the study has a high risk of bias.
Two studies [50] [37] compared cognitive therapy to respondent therapy, in the form of progressive relaxation training. Only one of these studies[37] reported on long-term pain and disability. These outcomes were not statistically significant between the groups. The review by Middelkoop et al. (2011)[56] also found these studies to have a high risk of bias.
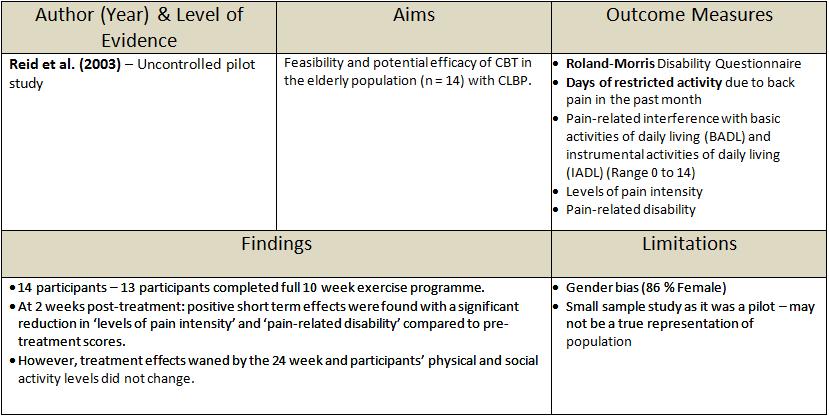
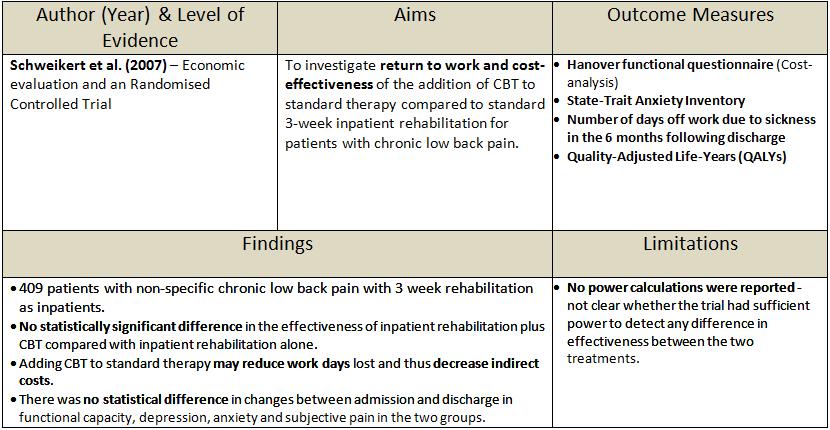
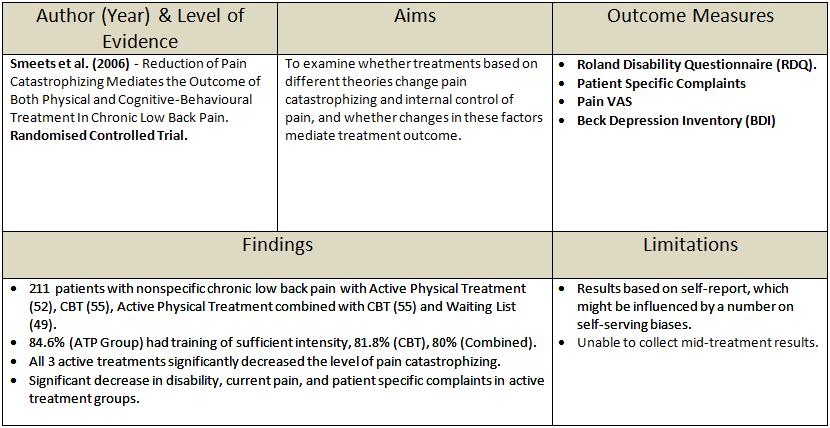
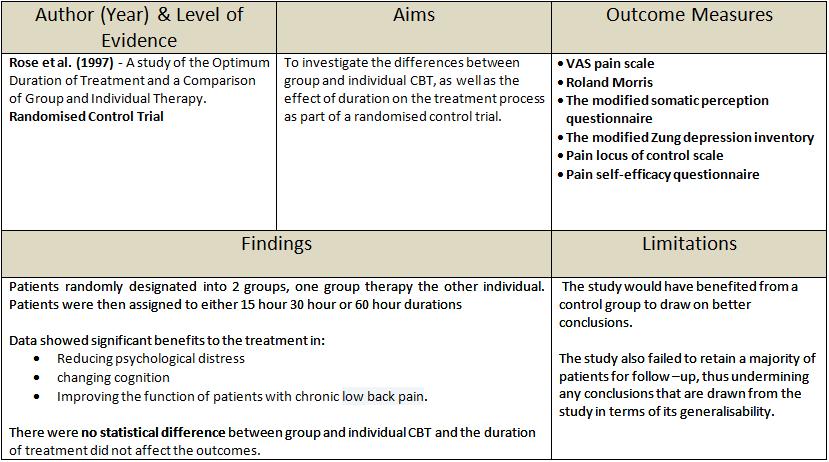
Cognitive Behavioral Therapy on Chronic Low Back Pain – The Evidence
Previous research has shown CBT to be an effective form of therapy on Chronic Low Back Pain (CLBP).
Negative Outcomes in Research
Positive Outcomes in Research
Candela Citations
- Cognitive Behavioral Therapy (CBT)u00a0. Located at: https://physio-pedia.com/CBT_Approach_to_Chronic_Low_Back_Pain?utm_source=physiopedia&utm_medium=related_articles&utm_campaign=ongoing_internal. License: CC BY-SA: Attribution-ShareAlike