Our emotions, thoughts, and behaviors play an important role in our health. Not only do they influence our day-to-day health practices, but they can also influence how our body functions. This module provides an overview of health psychology, which is a field devoted to understanding the connections between psychology and health. Discussed here are examples of topics a health psychologist might study, including stress, psychosocial factors related to health and disease, how to use psychology to improve health, and the role of psychology in medicine.
Learning Objectives
- Describe basic terminology used in the field of health psychology.
- Explain theoretical models of health, as well as the role of psychological stress in the development of disease.
- Describe psychological factors that contribute to resilience and improved health.
- Defend the relevance and importance of psychology to the field of medicine.
What Is Health Psychology?
Today, we face more chronic disease than ever before because we are living longer lives while also frequently behaving in unhealthy ways. One example of a chronic disease is coronary heart disease (CHD): It is the number one cause of death worldwide (World Health Organization, 2013). CHD develops slowly over time and typically appears midlife, but related heart problems can persist for years after the original diagnosis or cardiovascular event. In managing illnesses that persist over time (other examples might include cancer, diabetes, and long-term disability) many psychological factors will determine the progression of the ailment. For example, do patients seek help when appropriate? Do they follow doctor recommendations? Do they develop negative psychological symptoms due to lasting illness (e.g., depression)? Also important is that psychological factors can play a significant role in who develops these diseases, the prognosis, and the nature of the symptoms related to the illness. Health psychology is a relatively new, interdisciplinary field of study that focuses on these very issues, or more specifically, the role of psychology in maintaining health, as well as preventing and treating illness.

Consideration of how psychological and social factors influence health is especially important today because many of the leading causes of illness in developed countries are often attributed to psychological and behavioral factors. In the case of CHD, discussed above, psychosocial factors, such as excessive stress, smoking, unhealthy eating habits, and some personality traits can also lead to increased risk of disease and worse health outcomes. That being said, many of these factors can be adjusted using psychological techniques. For example, clinical health psychologists can improve health practices like poor dietary choices and smoking, they can teach important stress reduction techniques, and they can help treat psychological disorders tied to poor health. Health psychology considers how the choices we make, the behaviors we engage in, and even the emotions that we feel, can play an important role in our overall health (Cohen & Herbert, 1996; Taylor, 2012).
Health psychology relies on the Biopsychosocial Model of Health. This model posits that biology, psychology, and social factors are just as important in the development of disease as biological causes (e.g., germs, viruses), which is consistent with the World Health Organization (1946) definition of health. This model replaces the older Biomedical Model of Health, which primarily considers the physical, or pathogenic, factors contributing to illness. Thanks to advances in medical technology, there is a growing understanding of the physiology underlying the mind–body connection, and in particular, the role that different feelings can have on our body’s function. Health psychology researchers working in the fields of psychosomatic medicine and psychoneuroimmunology, for example, are interested in understanding how psychological factors can “get under the skin” and influence our physiology in order to better understand how factors like stress can make us sick.
Stress And Health
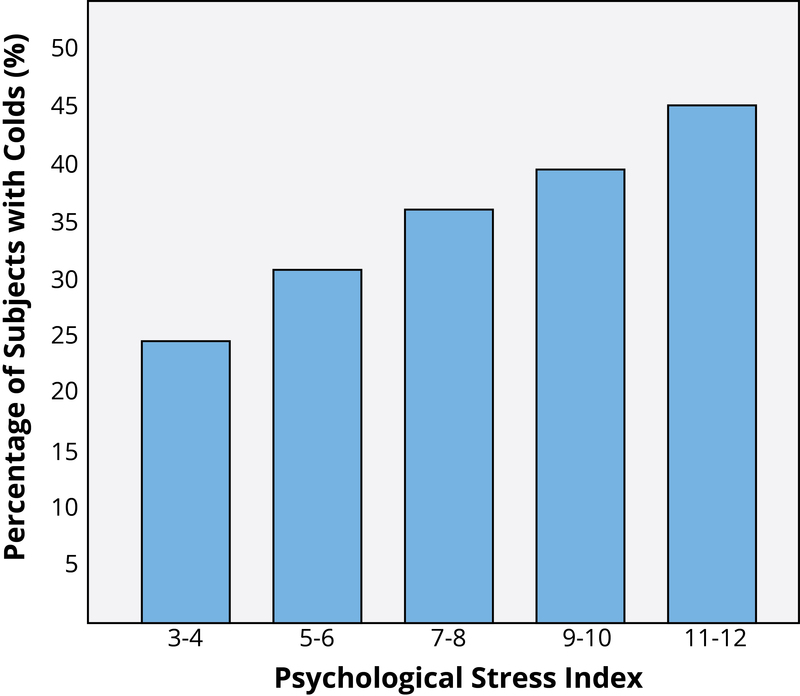
You probably know exactly what it’s like to feel stress, but what you may not know is that it can objectively influence your health. Answers to questions like, “How stressed do you feel?” or “How overwhelmed do you feel?” can predict your likelihood of developing both minor illnesses as well as serious problems like future heart attack (Cohen, Janicki-Deverts, & Miller, 2007). (Want to measure your own stress level? Check out the links at the end of the module.) To understand how health psychologists study these types of associations, we will describe one famous example of a stress and health study. Imagine that you are a research subject for a moment. After you check into a hotel room as part of the study, the researchers ask you to report your general levels of stress. Not too surprising; however, what happens next is that you receive droplets of cold virus into your nose! The researchers intentionally try to make you sick by exposing you to an infectious illness. After they expose you to the virus, the researchers will then evaluate you for several days by asking you questions about your symptoms, monitoring how much mucus you are producing by weighing your used tissues, and taking body fluid samples—all to see if you are objectively ill with a cold. Now, the interesting thing is that not everyone who has drops of cold virus put in their nose develops the illness. Studies like this one find that people who are less stressed and those who are more positive at the beginning of the study are at a decreased risk of developing a cold (Cohen, Tyrrell, & Smith, 1991; Cohen, Alper, Doyle, Treanor, & Turner, 2006) (see Figure 1 for an example).
Importantly, it is not just major life stressors (e.g., a family death, a natural disaster) that increase the likelihood of getting sick. Even small daily hassles like getting stuck in traffic or fighting with your girlfriend can raise your blood pressure, alter your stress hormones, and even suppress your immune system function (DeLongis, Folkman, & Lazarus, 1988; Twisk, Snel, Kemper, & van Machelen, 1999).
It is clear that stress plays a major role in our mental and physical health, but what exactly is it? The term stress was originally derived from the field of mechanics where it is used to describe materials under pressure. The word was first used in a psychological manner by researcher Hans Selye. He was examining the effect of an ovarian hormone that he thought caused sickness in a sample of rats. Surprisingly, he noticed that almost any injected hormone produced this same sickness. He smartly realized that it was not the hormone under investigation that was causing these problems, but instead, the aversive experience of being handled and injected by researchers that led to high physiological arousal and, eventually, to health problems like ulcers. Selye (1946) coined the term stressor to label a stimulus that had this effect on the body and developed a model of the stress response called the General Adaptation Syndrome. Since then, psychologists have studied stress in a myriad of ways, including stress as negative events (e.g., natural disasters or major life changes like dropping out of school), as chronically difficult situations (e.g., taking care of a loved one with Alzheimer’s), as short-term hassles, as a biological fight-or-flight response, and even as clinical illness like post-traumatic stress disorder (PTSD). It continues to be one of the most important and well-studied psychological correlates of illness, because excessive stress causes potentially damaging wear and tear on the body and can influence almost any imaginable disease process.
Protecting Our Health
An important question that health psychologists ask is: What keeps us protected from disease and alive longer? When considering this issue of resilience (Rutter, 1985), five factors are often studied in terms of their ability to protect (or sometimes harm) health. They are:
- Coping
- Control and Self-Efficacy
- Social Relationships
- Dispositions and Emotions
- Stress Management
Coping Strategies
How individuals cope with the stressors they face can have a significant impact on health. Coping is often classified into two categories: problem-focused coping or emotion-focused coping (Carver, Scheier, & Weintraub, 1989). Problem-focused coping is thought of as actively addressing the event that is causing stress in an effort to solve the issue at hand. For example, say you have an important exam coming up next week. A problem-focused strategy might be to spend additional time over the weekend studying to make sure you understand all of the material. Emotion-focused coping, on the other hand, regulates the emotions that come with stress. In the above examination example, this might mean watching a funny movie to take your mind off the anxiety you are feeling. In the short term, emotion-focused coping might reduce feelings of stress, but problem-focused coping seems to have the greatest impact on mental wellness (Billings & Moos, 1981; Herman-Stabl, Stemmler, & Petersen, 1995). That being said, when events are uncontrollable (e.g., the death of a loved one), emotion-focused coping directed at managing your feelings, at first, might be the better strategy. Therefore, it is always important to consider the match of the stressor to the coping strategy when evaluating its plausible benefits.
Control and Self-Efficacy

Another factor tied to better health outcomes and an improved ability to cope with stress is having the belief that you have control over a situation. For example, in one study where participants were forced to listen to unpleasant (stressful) noise, those who were led to believe that they had control over the noise performed much better on proofreading tasks afterwards (Glass & Singer, 1972). In other words, even though participants did not have actual control over the noise, the control belief aided them in completing the task. In similar studies, perceived control benefited immune system functioning (Sieber et al., 1992). Outside of the laboratory, studies have shown that older residents in assisted living facilities, which are notorious for low control, lived longer and showed better health outcomes when given control over something as simple as watering a plant or choosing when student volunteers came to visit (Rodin & Langer, 1977; Schulz & Hanusa, 1978). In addition, feeling in control of a threatening situation can actually change stress hormone levels (Dickerson & Kemeny, 2004). Believing that you have control over your own behaviors can also have a positive influence on important outcomes like smoking cessation, contraception use, and weight management (Wallston & Wallston, 1978). When individuals do not believe they have control, they do not try to change. Self-efficacy is closely related to control, in that people with high levels of this trait believe they can complete tasks and reach their goals. Just as feeling in control can reduce stress and improve health, higher self-efficacy can reduce stress and negative health behaviors, and is associated with better health (O’Leary, 1985).
Social Relationships
Research has shown that the impact of social isolation on our risk for disease and death is similar in magnitude to the risk associated with smoking regularly (Holt-Lunstad, Smith, & Layton, 2010; House, Landis, & Umberson, 1988). In fact, the importance of social relationships for our health is so significant that some scientists believe our body has developed a physiological system that encourages us to seek out our relationships, especially in times of stress (Taylor et al., 2000). Social integration is the concept used to describe the number of social roles that you have (Cohen & Wills, 1985), as well as the lack of isolation. For example, you might be a daughter, a basketball team member, a Humane Society volunteer, a coworker, and a student. Maintaining these different roles can improve your health via encouragement from those around you to maintain a healthy lifestyle. Those in your social network might also provide you with social support (e.g., when you are under stress). This support might include emotional help (e.g., a hug when you need it), tangible help (e.g., lending you money), or advice. By helping to improve health behaviors and reduce stress, social relationships can have a powerful, protective impact on health, and in some cases, might even help people with serious illnesses stay alive longer (Spiegel, Kraemer, Bloom, & Gottheil, 1989).
Dispositions and Emotions: What’s Risky and What’s Protective?
Negative dispositions and personality traits have been strongly tied to an array of health risks. One of the earliest negative trait-to-health connections was discovered in the 1950s by two cardiologists. They made the interesting discovery that there were common behavioral and psychological patterns among their heart patients that were not present in other patient samples. This pattern included being competitive, impatient, hostile, and time urgent. They labeled it Type A Behavior. Importantly, it was found to be associated with double the risk of heart disease as compared with Type B Behavior (Friedman & Rosenman, 1959). Since the 1950s, researchers have discovered that it is the hostility and competitiveness components of Type A that are especially harmful to heart health (Iribarren et al., 2000; Matthews, Glass, Rosenman, & Bortner, 1977; Miller, Smith, Turner, Guijarro, & Hallet, 1996). Hostile individuals are quick to get upset, and this angry arousal can damage the arteries of the heart. In addition, given their negative personality style, hostile people often lack a heath-protective supportive social network.
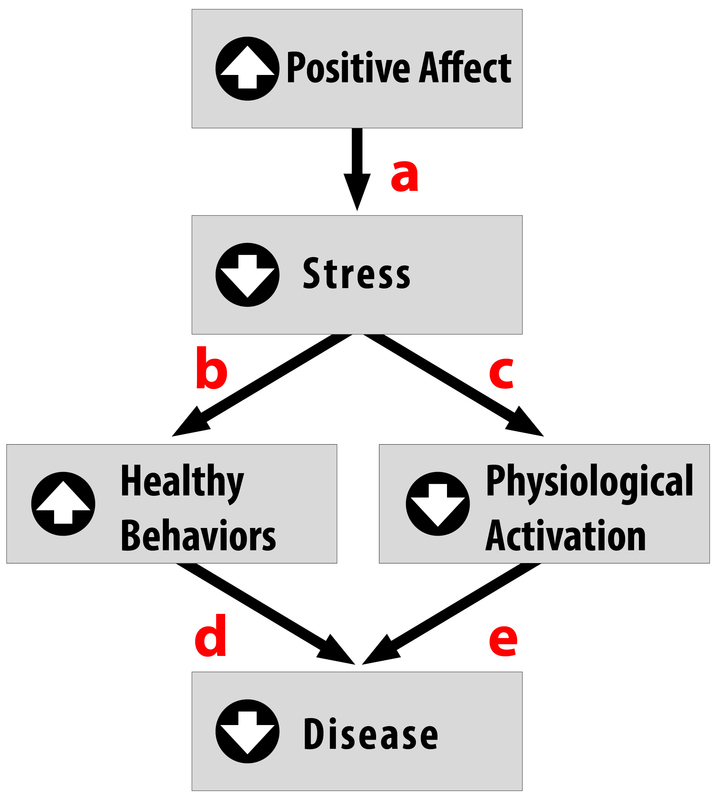
Positive traits and states, on the other hand, are often health protective. For example, characteristics like positive emotions (e.g., feeling happy or excited) have been tied to a wide range of benefits such as increased longevity, a reduced likelihood of developing some illnesses, and better outcomes once you are diagnosed with certain diseases (e.g., heart disease, HIV) (Pressman & Cohen, 2005). Across the world, even in the most poor and underdeveloped nations, positive emotions are consistently tied to better health (Pressman, Gallagher, & Lopez, 2013). Positive emotions can also serve as the “antidote” to stress, protecting us against some of its damaging effects (Fredrickson, 2001; Pressman & Cohen, 2005; see Figure 2). Similarly, looking on the bright side can also improve health. Optimism has been shown to improve coping, reduce stress, and predict better disease outcomes like recovering from a heart attack more rapidly (Kubzansky, Sparrow, Vokonas, & Kawachi, 2001; Nes & Segerstrom, 2006; Scheier & Carver, 1985; Segerstrom, Taylor, Kemeny, & Fahey, 1998).
Stress Management
About 20 percent of Americans report having stress, with 18–33 year-olds reporting the highest levels (American Psychological Association, 2012). Given that the sources of our stress are often difficult to change (e.g., personal finances, current job), a number of interventions have been designed to help reduce the aversive responses to duress. For example, relaxation activities and forms of meditation are techniques that allow individuals to reduce their stress via breathing exercises, muscle relaxation, and mental imagery. Physiological arousal from stress can also be reduced via biofeedback, a technique where the individual is shown bodily information that is not normally available to them (e.g., heart rate), and then taught strategies to alter this signal. This type of intervention has even shown promise in reducing heart and hypertension risk, as well as other serious conditions (e.g., Moravec, 2008; Patel, Marmot, & Terry, 1981). But reducing stress does not have to be complicated! For example, exercise is a great stress reduction activity (Salmon, 2001) that has a myriad of health benefits.
The Importance Of Good Health Practices
As a student, you probably strive to maintain good grades, to have an active social life, and to stay healthy (e.g., by getting enough sleep), but there is a popular joke about what it’s like to be in college: you can only pick two of these things (see Figure 3 for an example). The busy life of a college student doesn’t always allow you to maintain all three areas of your life, especially during test-taking periods. In one study, researchers found that students taking exams were more stressed and, thus, smoked more, drank more caffeine, had less physical activity, and had worse sleep habits (Oaten & Chang, 2005), all of which could have detrimental effects on their health. Positive health practices are especially important in times of stress when your immune system is compromised due to high stress and the elevated frequency of exposure to the illnesses of your fellow students in lecture halls, cafeterias, and dorms.
Psychologists study both health behaviors and health habits. The former are behaviors that can improve or harm your health. Some examples include regular exercise, flossing, and wearing sunscreen, versus negative behaviors like drunk driving, pulling all-nighters, or smoking. These behaviors become habits when they are firmly established and performed automatically. For example, do you have to think about putting your seatbelt on or do you do it automatically? Habits are often developed early in life thanks to parental encouragement or the influence of our peer group.
While these behaviors sound minor, studies have shown that those who engaged in more of these protective habits (e.g., getting 7–8 hours of sleep regularly, not smoking or drinking excessively, exercising) had fewer illnesses, felt better, and were less likely to die over a 9–12-year follow-up period (Belloc & Breslow 1972; Breslow & Enstrom 1980). For college students, health behaviors can even influence academic performance. For example, poor sleep quality and quantity are related to weaker learning capacity and academic performance (Curcio, Ferrara, & De Gennaro, 2006). Due to the effects that health behaviors can have, much effort is put forward by psychologists to understand how to change unhealthy behaviors, and to understand why individuals fail to act in healthy ways. Health promotion involves enabling individuals to improve health by focusing on behaviors that pose a risk for future illness, as well as spreading knowledge on existing risk factors. These might be genetic risks you are born with, or something you developed over time like obesity, which puts you at risk for Type 2 diabetes and heart disease, among other illnesses.
Psychology And Medicine
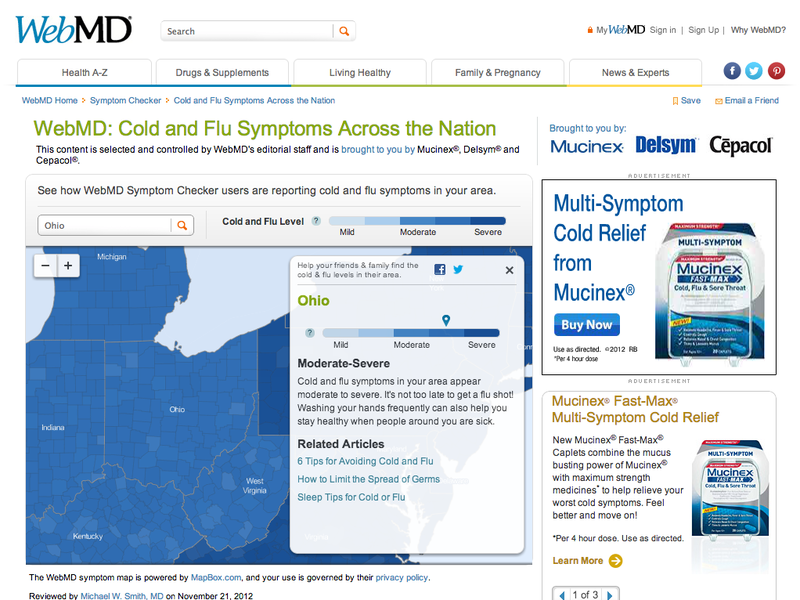
There are many psychological factors that influence medical treatment outcomes. For example, older individuals, (Meara, White, & Cutler, 2004), women (Briscoe, 1987), and those from higher socioeconomic backgrounds (Adamson, Ben-Shlomo, Chaturvedi, & Donovan, 2008) are all more likely to seek medical care. On the other hand, some individuals who need care might avoid it due to financial obstacles or preconceived notions about medical practitioners or the illness. Thanks to the growing amount of medical information online, many people now use the Internet for health information and 38% percent report that this influences their decision to see a doctor (Fox & Jones, 2009). Unfortunately, this is not always a good thing because individuals tend to do a poor job assessing the credibility of health information. For example, college-student participants reading online articles about HIV and syphilis rated a physician’s article and a college student’s article as equally credible if the participants said they were familiar with the health topic (Eastin, 2001). Credibility of health information often means how accurate or trustworthy the information is, and it can be influenced by irrelevant factors, such as the website’s design, logos, or the organization’s contact information (Freeman & Spyridakis, 2004). Similarly, many people post health questions on online, unmoderated forums where anyone can respond, which allows for the possibility of inaccurate information being provided for serious medical conditions by unqualified individuals.
After individuals decide to seek care, there is also variability in the information they give their medical provider. Poor communication (e.g., due to embarrassment or feeling rushed) can influence the accuracy of the diagnosis and the effectiveness of the prescribed treatment. Similarly, there is variation following a visit to the doctor. While most individuals are tasked with a health recommendation (e.g., buying and using a medication appropriately, losing weight, going to another expert), not everyone adheres to medical recommendations (Dunbar-Jacob & Mortimer-Stephens, 2010). For example, many individuals take medications inappropriately (e.g., stopping early, not filling prescriptions) or fail to change their behaviors (e.g., quitting smoking). Unfortunately, getting patients to follow medical orders is not as easy as one would think. For example, in one study, over one third of diabetic patients failed to get proper medical care that would prevent or slow down diabetes-related blindness (Schoenfeld, Greene, Wu, & Leske, 2001)! Fortunately, as mobile technology improves, physicians now have the ability to monitor adherence and work to improve it (e.g., with pill bottles that monitor if they are opened at the right time). Even text messages are useful for improving treatment adherence and outcomes in depression, smoking cessation, and weight loss (Cole-Lewis, & Kershaw, 2010).
Being A Health Psychologist
Training as a clinical health psychologist provides a variety of possible career options. Clinical health psychologists often work on teams of physicians, social workers, allied health professionals, and religious leaders. These teams may be formed in locations like rehabilitation centers, hospitals, primary care offices, emergency care centers, or in chronic illness clinics. Work in each of these settings will pose unique challenges in patient care, but the primary responsibility will be the same. Clinical health psychologists will evaluate physical, personal, and environmental factors contributing to illness and preventing improved health. In doing so, they will then help create a treatment strategy that takes into account all dimensions of a person’s life and health, which maximizes its potential for success. Those who specialize in health psychology can also conduct research to discover new health predictors and risk factors, or develop interventions to prevent and treat illness. Researchers studying health psychology work in numerous locations, such as universities, public health departments, hospitals, and private organizations. In the related field of behavioral medicine, careers focus on the application of this type of research. Occupations in this area might include jobs in occupational therapy, rehabilitation, or preventative medicine. Training as a health psychologist provides a wide skill set applicable in a number of different professional settings and career paths.
The Future Of Health Psychology
Much of the past medical research literature provides an incomplete picture of human health. “Health care” is often “illness care.” That is, it focuses on the management of symptoms and illnesses as they arise. As a result, in many developed countries, we are faced with several health epidemics that are difficult and costly to treat. These include obesity, diabetes, and cardiovascular disease, to name a few. The National Institutes of Health have called for researchers to use the knowledge we have about risk factors to design effective interventions to reduce the prevalence of preventable illness. Additionally, there are a growing number of individuals across developed countries with multiple chronic illnesses and/or lasting disabilities, especially with older age. Addressing their needs and maintaining their quality of life will require skilled individuals who understand how to properly treat these populations. Health psychologists will be on the forefront of work in these areas.
With this focus on prevention, it is important that health psychologists move beyond studying risk (e.g., depression, stress, hostility, low socioeconomic status) in isolation, and move toward studying factors that confer resilience and protection from disease. There is, fortunately, a growing interest in studying the positive factors that protect our health (e.g., Diener & Chan, 2011; Pressman & Cohen, 2005; Richman, Kubzansky, Maselko, Kawachi, Choo, & Bauer, 2005) with evidence strongly indicating that people with higher positivity live longer, suffer fewer illnesses, and generally feel better. Seligman (2008) has even proposed a field of “Positive Health” to specifically study those who exhibit “above average” health—something we do not think about enough. By shifting some of the research focus to identifying and understanding these health-promoting factors, we may capitalize on this information to improve public health.
Innovative interventions to improve health are already in use and continue to be studied. With recent advances in technology, we are starting to see great strides made to improve health with the aid of computational tools. For example, there are hundreds of simple applications (apps) that use email and text messages to send reminders to take medication, as well as mobile apps that allow us to monitor our exercise levels and food intake (in the growing mobile-health, or m-health, field). These m-health applications can be used to raise health awareness, support treatment and compliance, and remotely collect data on a variety of outcomes. Also exciting are devices that allow us to monitor physiology in real time; for example, to better understand the stressful situations that raise blood pressure or heart rate. With advances like these, health psychologists will be able to serve the population better, learn more about health and health behavior, and develop excellent health-improving strategies that could be specifically targeted to certain populations or individuals. These leaps in equipment development, partnered with growing health psychology knowledge and exciting advances in neuroscience and genetic research, will lead health researchers and practitioners into an exciting new time where, hopefully, we will understand more and more about how to keep people healthy.
DISCUSSION QUESTIONS
- What psychological factors contribute to health?
- Which psychosocial constructs and behaviors might help protect us from the damaging effects of stress?
- What kinds of interventions might help to improve resilience? Who will these interventions help the most?
- How should doctors use research in health psychology when meeting with patients?
- Why do clinical health psychologists play a critical role in improving public health?
Key Takeaways
- Adherence
- In health, it is the ability of a patient to maintain a health behavior prescribed by a physician. This might include taking medication as prescribed, exercising more, or eating less high-fat food.
- Behavioral medicine
- A field similar to health psychology that integrates psychological factors (e.g., emotion, behavior, cognition, and social factors) in the treatment of disease. This applied field includes clinical areas of study, such as occupational therapy, hypnosis, rehabilitation or medicine, and preventative medicine.
- Biofeedback
- The process by which physiological signals, not normally available to human perception, are transformed into easy-to-understand graphs or numbers. Individuals can then use this information to try to change bodily functioning (e.g., lower blood pressure, reduce muscle tension).
- Biomedical Model of Health
- A reductionist model that posits that ill health is a result of a deviation from normal function, which is explained by the presence of pathogens, injury, or genetic abnormality.
- An approach to studying health and human function that posits the importance of biological, psychological, and social (or environmental) processes.
- Chronic disease
- A health condition that persists over time, typically for periods longer than three months (e.g., HIV, asthma, diabetes).
- Control
- Feeling like you have the power to change your environment or behavior if you need or want to.
- Daily hassles
- Irritations in daily life that are not necessarily traumatic, but that cause difficulties and repeated stress.
- Emotion-focused coping
- Coping strategy aimed at reducing the negative emotions associated with a stressful event.
- General Adaptation Syndrome
- A three-phase model of stress, which includes a mobilization of physiological resources phase, a coping phase, and an exhaustion phase (i.e., when an organism fails to cope with the stress adequately and depletes its resources).
- Health
- According to the World Health Organization, it is a complete state of physical, mental, and social well-being and not merely the absence of disease or infirmity.
- Health behavior
- Any behavior that is related to health—either good or bad.
- Hostility
- An experience or trait with cognitive, behavioral, and emotional components. It often includes cynical thoughts, feelings of emotion, and aggressive behavior.
- Mind–body connection
- The idea that our emotions and thoughts can affect how our body functions.
- Problem-focused coping
- A set of coping strategies aimed at improving or changing stressful situations.
- Psychoneuroimmunology
- A field of study examining the relationship among psychology, brain function, and immune function.
- Psychosomatic medicine
- An interdisciplinary field of study that focuses on how biological, psychological, and social processes contribute to physiological changes in the body and health over time.
- Resilience
- The ability to “bounce back” from negative situations (e.g., illness, stress) to normal functioning or to simply not show poor outcomes in the face of adversity. In some cases, resilience may lead to better functioning following the negative experience (e.g., post-traumatic growth).
- Self-efficacy
- The belief that one can perform adequately in a specific situation.
- The size of your social network, or number of social roles (e.g., son, sister, student, employee, team member).
- The perception or actuality that we have a social network that can help us in times of need and provide us with a variety of useful resources (e.g., advice, love, money).
- Stress
- A pattern of physical and psychological responses in an organism after it perceives a threatening event that disturbs its homeostasis and taxes its abilities to cope with the event.
- Stressor
- An event or stimulus that induces feelings of stress.
- Type A Behavior
- Type A behavior is characterized by impatience, competitiveness, neuroticism, hostility, and anger.
- Type B Behavior
- Type B behavior reflects the absence of Type A characteristics and is represented by less competitive, aggressive, and hostile behavior patterns.
Candela Citations
- The Healthy Life by Emily Hooker and Sarah Pressman is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. . Authored by: Hooker, E. & Pressman, S. (2021). The healthy life. In R. Biswas-Diener & E. Diener (Eds), Noba textbook series: Psychology. Champaign, IL: DEF publishers.. Located at: http://noba.to/4tm85z2x. License: CC BY-NC-SA: Attribution-NonCommercial-ShareAlike
